Approach
A focused, problem-oriented history and a thorough physical examination are essential to narrow down the differential diagnoses, streamline appropriate investigations, and establish the cause of the joint inflammation in a given patient. It is important to ascertain the correct diagnosis before initiating definitive treatment, as the wrong diagnosis and incorrect treatment can lead to irreversible joint damage.
A significant number of people have undifferentiated peripheral inflammatory arthritis (UPIA) for which no underlying cause can be found on initial investigation.[40][41][42] Over time, UPIA may either persist in these patients, or may progress to a specific diagnosis, or even enter remission. It is important to monitor disease activity in these patients.[4][40][41]
History and physical examination
The differential diagnosis of joint inflammation will depend on whether the inflammation is acute and confined to a single joint, or whether it involves multiple joints. The physician should keep in mind the caveat that most causes of oligo- or polyarthritis can also be causes of monoarthritis, because almost any arthritic condition can initially affect a single joint.
Acute monoarthropathy
When a patient presents with an acute hot monoarthropathy, one must consider and exclude septic (pyogenic) arthritis. Septic (pyogenic) non-gonococcal arthritis most commonly affects:
Older people
Intravenous drug users
Those with recent bacteraemia
People with diabetes
Immunocompromised patients (e.g., those with HIV disease, on chemotherapy or other immunosuppressive drugs, or immunodeficient states)
Patients with sickle cell disease or other haemoglobinopathies
People with rheumatoid arthritis (RA)
Those with prosthetic joints.
A typical history might include recent bacteraemia, skin infection, or joint surgery, and the presence of prosthetic joints. Acute onset of swelling, with severe pain and very limited range of motion in a single joint or, rarely, in a few joints, is accompanied by constitutional features such as fever and malaise. The knee joint is affected in 50% of patients.[43] Identification of bacteria in the synovial fluid by Gram stain, with subsequent recovery of the organism on culture, is the definitive diagnostic test. If synovial fluid cannot be obtained with closed needle aspiration, the joint should be aspirated under computed tomography (CT) or ultrasound guidance.
Other conditions presenting with acute monoarthritis include gonococcal arthritis, acute gout, acute pseudogout, haemarthrosis with or without joint trauma, a monoarticular presentation of reactive arthritis, Lyme arthritis, tenosynovial giant cell tumour (formerly, pigmented villonodular synovitis), synovial osteochondromatosis, and lipoma arborescens.
Disseminated gonococcal infection (DGI) occurs in 0.5% to 3% of patients infected with Neisseria gonorrhoeae. It presents with fever, chills, malaise, and mono- or polyarthralgia, along with tenosynovitis (wrists, fingers, ankles, toes) and sparse (between 2 and 10) pustular or vesiculo-pustular skin lesions.[44] These skin lesions may be subtle and missed unless specifically looked for. Mono- or oligoarthritis resulting from DGI typically affects the knees, wrists, or ankles. Pain along tendon sheaths with active or passive joint movement is a feature of gonococcal tenosynovitis. Blood and synovial fluid culture on Thayer-Martin medium can grow N gonorrhoeae.
Clinical gout comprises a heterogeneous group of disorders characterised by deposition of monosodium urate (MSU) crystals in the joints and tendons.[31] The usual manifestations of acute gout are severe pain, redness, and swelling involving a single joint (approximately 80% of patients), often in the lower extremity, typically at the first metatarso-phalangeal joint (podagra). Maximal severity of the attack is usually reached over several hours. Even if untreated, the episode almost always resolves completely within a few days to several weeks. Long-standing gouty arthropathy is often associated with tophaceous deposits. Under polarised light microscopy, MSU crystals (both intra- and extra-cellular) are visible in the synovial fluid aspirate and in an aspirate from a tophus.[45][46][Figure caption and citation for the preceding image starts]: Tophaceous goutFrom the collection of Dr Soumya Chatterjee [Citation ends].
 [Figure caption and citation for the preceding image starts]: Monosodium urate crystals from a tophus (polarised light microscopy)From the collection of Dr Soumya Chatterjee [Citation ends].
[Figure caption and citation for the preceding image starts]: Monosodium urate crystals from a tophus (polarised light microscopy)From the collection of Dr Soumya Chatterjee [Citation ends].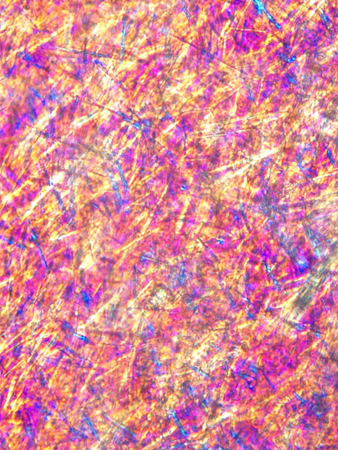
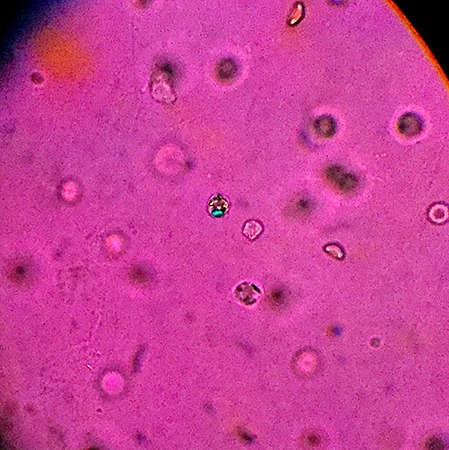
Acute pseudogout results from crystal precipitation of calcium pyrophosphate dihydrate (CPPD). CPPD crystal-induced synovitis can clinically resemble gout: self-limiting acute or subacute attacks of mono- or oligoarthritis (involving <5 joints).[47] Trauma, surgery, or medical illness can precipitate these attacks. The typical patient is >65 years old, with a history of recurrent episodes of arthritis. The knee is affected in >50% of patients, although attacks may also involve the wrists, metacarpo-phalangeal (MCP) joints, shoulders, and elbows. A symmetrical pattern of joint involvement is common, but unilateral involvement may also occur. Chondrocalcinosis (presence of calcification in fibrocartilage and hyaline cartilage that is visible on x-ray) is commonly present in patients with CPPD crystal deposition disease. Disorders associated with CPPD deposition disease include haemochromatosis, hyperparathyroidism, hypomagnesaemia, hypophosphatasia, hypothyroidism, and familial hypocalciuric hypercalcaemia.[48] Screening for associated diseases should be guided by the clinical presentation and level of suspicion.[49][Figure caption and citation for the preceding image starts]: Calcium pyrophosphate dihydrate (CPPD) crystals in synovial fluid under compensated polarised light microscopyFrom the collection of Dr Soumya Chatterjee [Citation ends].
 [Figure caption and citation for the preceding image starts]: Chondrocalcinosis (lateral meniscus of left knee)From the collection of Dr Soumya Chatterjee [Citation ends].
[Figure caption and citation for the preceding image starts]: Chondrocalcinosis (lateral meniscus of left knee)From the collection of Dr Soumya Chatterjee [Citation ends]. A familial form of CPPD disease has been associated with ANKH gene mutation.[50][51]
A familial form of CPPD disease has been associated with ANKH gene mutation.[50][51]Bleeding into a joint (haemarthrosis) is an important cause of monoarticular joint pain and swelling. Factors that may influence haemarthrosis include trauma, bleeding disorders (haemophilia), neurological deficits (Charcot's joint), intra-articular neoplasms (e.g., tenosynovial giant cell tumour), or a vascular abnormality (haemangioma, arteriovenous malformation, aneurysm, synovial vascular structural anomalies). The joint is swollen and warm, and has a very painful and restricted range of motion. Superficial bruising and ecchymoses can be seen. Lipohaemarthrosis, due to leakage of marrow fat into the synovial fluid, strongly suggests an intra-articular fracture. Bloody effusion in haemarthrosis usually fails to clot due to chronic fibrinolysis, while blood from a traumatic aspiration generally clots. X-ray of the affected joint may identify an intracapsular fracture, whereas a magnetic resonance imaging (MRI) scan is necessary to demonstrate injury to the cartilage, intra-articular ligament rupture, or tenosynovial giant cell tumour.
Traumatic synovial effusion is suggested by history, and should prompt immobilisation and appropriate imaging studies to rule out any anatomical abnormalities.
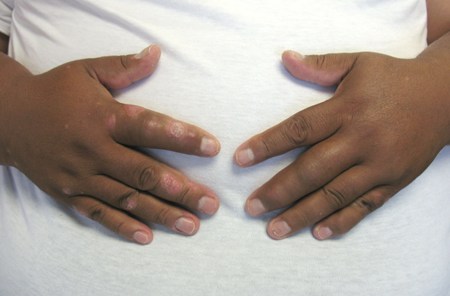
Reactive arthritis develops soon after an infection elsewhere in the body, but the microorganisms cannot be recovered from the joint. The classic pathogens in reactive arthritis are Chlamydia trachomatis, Chlamydia pneumoniae, Yersinia, Salmonella, Shigella, Campylobacter, Clostridium difficile, and bacillus Calmette-Guérin (BCG, following intravesical instillation in the treatment of bladder cancer). The lag period between the preceding symptomatic infection and onset of arthritis ranges from several days to several weeks. The typical presentation is an asymmetrical mono- or oligoarthritis (involving <5 joints), which predominantly affects the lower extremities. However, about 50% of patients also have arthritis in the upper extremities, and some have small joint polyarthritis. Dactylitis, enthesitis, and tenosynovitis may be present. Extra-articular manifestations include conjunctivitis and anterior uveitis, oral ulcers, urethritis, keratoderma blennorrhagicum (psoriasiform skin changes on the soles of the feet), nail changes similar to psoriasis, and circinate balanitis. Urethritis can cause dysuria and pelvic pain. Infections by Yersinia, Salmonella, Campylobacter, andC pneumoniae cause strong antibody responses. IgM and rising IgG titres (paired sera) may be useful in diagnosis of recent Yersinia and Campylobacter infections, even in communities where seroprevalence is high. HLA-B27 testing is not useful for the diagnosis of reactive arthritis irrespective of prior probability. However, it is useful prognostically in that HLA-B27-positive patients have more severe and prolonged duration of arthritis and are more likely to develop chronic spondyloarthritis. Reactive arthritis can behave more aggressively in patients with co-existing HIV disease.[Figure caption and citation for the preceding image starts]: Dactylitis of right third toe (reactive arthritis)From the collection of Dr Soumya Chatterjee [Citation ends].

Lyme disease, caused by an infected tick bite (Ixodes species), is now the most common vector-borne illness in the northern hemisphere.[52] Joint manifestations usually arise late in the course of the disease and are characterised by recurrent attacks of asymmetrical swelling and pain in a few large joints. A detailed travel and activity history, with enquiries about prior residences and prior clinical findings that might be consistent with Lyme disease, is important.[53] Intermittent mono- or oligoarthritis (involving <5 joints) occurs in about 60% of untreated patients with late disseminated disease; about 10% of untreated patients develop persistent monoarthritis. An antecedent bull's eye rash (erythema migrans) develops at the site of the tick bite in up to 85% of patients. The most commonly involved joints are the knee, shoulder, ankle, elbow, temporomandibular joint, and wrist.
Tenosynovial giant cell tumour occurs predominantly in young and middle-aged adults. This benign disorder is characterised by synovial hypertrophy, most commonly in the knee joint, with diffuse intra-articular haemosiderin deposition.
In synovial chondromatosis, loose cartilaginous bodies develop that may ossify in 70% to 95% of patients (osteochondromatosis). It mostly affects men and also commonly affects the knee joint.
Lipoma arborescens is characterised by benign lipomatous proliferation of the synovium, most often of the knee joint. This idiopathic condition is more common in men in the fourth and fifth decades.
Acute polyarthropathy
Causes of acute polyarthritis include RA, systemic lupus erythematosus (SLE), psoriatic arthritis, enteropathic arthritides (e.g., ulcerative colitis, Crohn's disease, coeliac disease, Whipple’s disease), reactive arthritis (note that this condition is also a cause of acute monoarthritis), Lyme disease (also a cause of acute monoarthritis), SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis), adult-onset Still's disease (AOSD), ankylosing spondylitis (AS), acute rheumatic fever (ARF), sarcoidosis, parvovirus B19 syndrome, paraneoplastic articular syndromes, arbovirus infections (such as chikungunya), remitting seronegative symmetrical synovitis with pitting oedema (RS3PE), and drug-induced acute polyarthritis.
RA is characterised by pain, swelling, and stiffness of the MCP and proximal inter-phalangeal (PIP) joints of both hands, as well as peripheral polyarthritis involving the wrists, elbows, shoulders, knees, ankles, and metatarso-phalangeal joints. Morning stiffness for at least 30 to 60 minutes is typical. Rheumatoid nodules tend to occur later in the course of the disease. Serum rheumatoid factor (RF) and antibodies to cyclic citrullinated peptides (CCP) are positive. The sensitivity of RF for the disease is 26%, with a specificity of 60%.[54] Anti-CCP antibodies have a higher sensitivity and specificity for RA, at 99.4% and 66%, respectively.[55][56] Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) indicate active joint inflammation. Characteristic marginal erosions of cartilage and bone around the MCP and PIP joints can be seen on x-ray of the hands, with severe subluxations and joint damage in advanced cases. Classification criteria for rheumatoid arthritis developed by the American College of Rheumatology/European League Against Rheumatism focus attention on earlier diagnosis and treatment.[57][58][59][Figure caption and citation for the preceding image starts]: Rheumatoid nodulesFrom the collection of Dr Soumya Chatterjee [Citation ends].
 [Figure caption and citation for the preceding image starts]: Rheumatoid hand x-rayFrom the collection of Dr Soumya Chatterjee [Citation ends].
[Figure caption and citation for the preceding image starts]: Rheumatoid hand x-rayFrom the collection of Dr Soumya Chatterjee [Citation ends]. [Figure caption and citation for the preceding image starts]: Rheumatoid arthritis (chronic hand deformities)From the collection of Dr Soumya Chatterjee [Citation ends].
[Figure caption and citation for the preceding image starts]: Rheumatoid arthritis (chronic hand deformities)From the collection of Dr Soumya Chatterjee [Citation ends].
SLE is a chronic autoimmune inflammatory disease that can affect the skin, joints, kidneys, lungs, nervous system, and serous membranes.[60] Young women (aged 20-30 years) are most frequently affected. Joint symptoms occur in over 90% of patients at some point and are often the earliest manifestation. Arthritis tends to be migratory and asymmetrical. Rarely, a progressively deforming, but reducible arthropathy (consisting mainly of ulnar deviation of the fingers at the MCP joints, called Jaccoud's arthropathy) can develop. Antinuclear antibody (ANA) is positive in significant titre (usually ≥1:160) in nearly all patients with SLE. This is the best diagnostic test, with high sensitivity, and should be performed whenever SLE is suspected.[61] A positive ANA (at a titre of ≥1:80 on HEp-2 cells or an equivalent positive test at least once) is a required (entry) criterion for the 2019 European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) Classification Criteria for SLE.[62] Antibodies to double-stranded DNA and anti-Smith (Sm) antibodies are also highly specific for SLE.[63][64]
Patients with psoriatic arthritis present with pain, swelling, and stiffness in the affected joints, with morning stiffness lasting >30 minutes in 50% of patients. The most frequent presentation is oligoarthritis (involving <5 joints). Dactylitis (sausage digit), enthesitis (inflammation of the entheses, the location where a bone has an insertion of a tendon or a ligament), and tenosynovitis are not uncommon.[16] The distal inter-phalangeal (DIP) joints and spine are affected in 40% to 50% of patients. Cutaneous psoriasis is present in 90% of cases.[65] Nail psoriasis can also be seen. DIP joint arthritis and arthritis mutilans (an extremely severe form of chronic destructive arthritis, characterised by resorption of bones and the consequent collapse of soft tissue leading to pencil-in-cup deformity and telescoping digits) can be seen in psoriatic arthritis. Psoriatic arthritis can behave more aggressively in patients with co-existing HIV disease. The Classification Criteria for Psoriatic Arthritis (CASPAR) study group has developed a validated set of classification criteria for psoriatic arthritis with a sensitivity of 91.4% and a specificity of 98.7%.[66][67][Figure caption and citation for the preceding image starts]: Psoriatic arthritis with dactylitis (left middle and right index finger); skin and nail changes (left ring finger)From the collection of Dr Soumya Chatterjee [Citation ends].
Enteropathic arthritides: these conditions lead to an inflammatory arthritis secondary to an immune-mediated process affecting the gastrointestinal tract. Examples include:
Inflammatory arthritis associated with inflammatory bowel disease (i.e., ulcerative colitis and Crohn's disease)
Reactive arthritis following infection with enteric pathogens such as Salmonella, Shigella, Campylobacter, Yersinia, Chlamydia, and Clostridium difficile (described above under 'reactive arthritis')
Inflammatory arthritis associated with intestinal bypass procedures (also known as bowel-associated dermatosis arthritis syndrome)
Coeliac disease
Whipple's disease (caused by a Gram-positive bacterium, Tropheryma whipplei).
Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome has some clinical manifestations that resemble psoriatic arthritis. Sterno-clavicular joint arthritis is a characteristic feature. Osteitis is the most prominent skeletal lesion, but lytic, sclerotic, and hyperostotic bone lesions also develop. Palmo-plantar pustulosis and acne are the main skin lesions.[68]
Inflammatory arthritis similar to reactive arthritis has been described in association with acne conglobata, hidradenitis suppurativa, and dissecting cellulitis of the scalp (follicular occlusion triad).
Monoarthritis of the knee is the most common rheumatological manifestation of late disseminated Lyme disease, but an asymmetrical large joint oligoarthritis (<5 joints) can also develop.
AOSD presents with polyarthralgia or a severe polyarthritis. This may be accompanied by severe muscle pain. In addition, there is a febrile rash that is non-pruritic, macular or maculo-papular, salmon coloured, and usually found over the trunk or extremities. A severe, non-suppurative pharyngitis is also common in AOSD and may presage disease relapses. Pericarditis, pleural effusions, and transient pulmonary infiltrates occur in 30% to 40% of patients.[69][70] Fusion of the wrist joints is characteristic of AOSD, although it occurs in only a minority of patients.[71] Serum ferritin concentration > 6741 picomol/L (>3000 nanograms/mL) is common in AOSD, with some patients having values >22,470 picomol/L (>10,000 nanograms/mL).[72] The elevation of ferritin correlates with disease activity. Bone marrow examination demonstrates pathognomonic evidence of macrophage activation syndrome (haemophagocytosis) in 12% of patients, with numerous, well-differentiated macrophages (histiocytes) that are involved in the phagocytosis of haematopoietic elements.[72]
AS is a chronic inflammatory disease of the axial skeleton, presenting with low back pain, sacroiliitis, and progressive stiffness of the spine. It characteristically affects young adults, with a peak age of onset between 20 and 30 years.[73] In 75% of patients, the first symptom is low back pain for >3 months: a constant dull ache in the low back, gluteal regions, and posterior thighs that typically improves with exercise but not with rest (as opposed to mechanical back pain), may awaken the patient from sleep, and is associated with morning stiffness of >30 minutes' duration. Groin pain (indicating hip arthritis), shoulder pain, and shoulder stiffness are common. Less commonly, other peripheral joints are affected. Costochondral, manubriosternal, sterno-clavicular, and costovertebral joints can also be affected. Another possible sign is enthesitis, which can manifest as Achilles' tendinitis or plantar fasciitis. Limited range of motion and pain on movement of the hips and shoulders is common. AS can co-exist with psoriasis and inflammatory bowel disease. Extra-articular manifestations include acute unilateral anterior uveitis, aortic valve disease, cardiac conduction abnormalities, and apical pulmonary fibrosis. Among white people, HLA-B27 is present in 95% of AS patients, compared with 8% of the general population.[74] HLA-B27 is more useful than x-rays for diagnosis in patients who have chronic low back pain, where a positive result for HLA-B27 is associated with a 30% to 60% chance of having AS.[74] Even after 10 years of AS, only 40% of patients have radiographic evidence of sacroiliitis on plain films.[75] MRI is the most sensitive and specific test in detecting the changes of sacroiliitis. It is indicated when plain x-rays are normal, but suspicion of AS is high (known as ‘non-radiographic axial spondyloarthritis’). For these early cases, MRI has a sensitivity of 60%.[76] Based on its performance in evaluating patients presenting with peripheral arthritis, enthesitis, and/or dactylitis, classification criteria for peripheral spondyloarthritis have been developed by the Assessment of SpondyloArthritis international Society (ASAS).[77]
Acute rheumatic fever (ARF) is a delayed, non-suppurative sequela of group A Streptococcus tonsillo-pharyngitis. There is usually a latent period of 2 to 3 weeks following pharyngitis before the first manifestations of ARF appear.[78] An acute migratory arthritis may develop affecting the knees, ankles, elbows, and wrists. The lower extremity joints are typically involved first. Streptococcal antibodies are most useful in diagnosis, as they reach a peak titre at about the time of onset of ARF, and indicate true infection rather than carriage. Other manifestations may include endocarditis, chorea, subcutaneous nodules, and erythema marginatum (Jones criteria).[79]
Sarcoidosis is a multi-system disorder of unknown aetiology. It typically affects young adults 20 to 40 years old, and may present with bilateral hilar and right paratracheal lymphadenopathy, pulmonary infiltrates, and skin or eye lesions (anterior and/or posterior uveitis). About 25% of patients develop sarcoid arthropathy.[80] Diagnosis may be difficult when a patient presents solely with joint pain. Löfgren's syndrome is characterised by the triad of bilateral hilar adenopathy, acute polyarthritis, and erythema nodosum. Although it is usually self-limiting, about one third of patients have a more persistent course. Chronic sarcoid arthropathy is frequently associated with interstitial lung disease and elevated angiotensin-converting enzyme levels.[81] In the presence of typical pulmonary or other extrapulmonary features of sarcoidosis, synovial histology revealing multiple non-caseating granulomata supports the diagnosis.[Figure caption and citation for the preceding image starts]: Erythema nodosumFrom the collection of Dr Soumya Chatterjee [Citation ends].

Symptoms are usually symmetrical and in multiple joints after parvovirus infection, and may mimic RA. The diagnosis is suggested by a viral prodrome with flu-like symptoms, and a rash (in some patients), shortly prior to joint inflammation.[82]
Paraneoplastic articular syndromes include hypertrophic osteoarthropathy, palmar fasciitis with polyarthritis syndrome, and paraneoplastic arthritis.[33][34]
In patients with inflammatory polyarthritis who have a history of travel to endemic areas, arbovirus infections such as chikungunya should be suspected. Patients may develop fever, a rash, myalgias, headache, and arthralgias 2 to 10 days after a mosquito bite (typically Aedes albopictus), and arthritis involves small joints of hands and feet, wrists, and ankles in the majority of those affected. About half of the patients continue to have arthritis 6 months after the onset of the disease. Diagnosis is made by viral culture or reverse transcriptase polymerase chain reaction (PCR) from an acute-phase specimen of serum.
Remitting seronegative symmetrical synovitis with pitting oedema (RS3PE) syndrome presents with acute-onset polyarthritis, with significant pitting oedema of the dorsal surfaces of the hands and feet. It is more commonly seen in males, in older patients (≥50 years), and is usually non-erosive. As the name implies, rheumatoid factor is negative.[21]
A detailed drug history is important in patients with an immune-mediated inflammatory arthropathy. Use of certain drugs, such as procainamide, hydralazine, minocycline, isoniazid, propylthiouracil, and tumour necrosis factor inhibitors can be associated with drug-induced lupus. Serum sickness-like reaction can be seen with various oral and parenteral pharmacological agents, including plasma-derived products and biological response modifiers (e.g., infliximab and rituximab). In addition, arthralgia, inflammatory arthritis, and tendinitis have also been associated with the use of aromatase inhibitors (e.g., anastrozole and letrozole), clopidogrel, quinolone antibiotics (e.g., levofloxacin and ciprofloxacin), statins, and dipeptidyl peptidase (DPP)-4 inhibitors (e.g., sitagliptin and saxagliptin).[25] Immune-related adverse events, including inflammatory arthritis, have been reported secondary to immune checkpoint inhibitor therapy for cancer.[26][27][28][29] In one case series of 13 patients treated with ipilimumab (anti-CTLA-4) and/or nivolumab (anti-PD-1) for solid tumours, 9 patients developed inflammatory arthritis (primarily polyarticular arthritis involving small and large joints similar to rheumatoid arthritis), and 4 had sicca symptoms.[83]
Laboratory investigations
The choice of laboratory investigations required varies according to the suspected differential diagnosis.
Septic arthritis
Definitive diagnosis of a septic joint requires joint aspiration and synovial fluid analysis (including Gram stain and culture).
Culture for gonococci on Thayer-Martin medium should be requested in suspected DGI. All patients with DGI should undergo assessment for concomitant Chlamydia, syphilis, and HIV infections. If urethritis is simultaneously present, a Gram stain of the urethral exudate should be obtained.
Gout and pseudogout
US guidelines recommend synovial fluid analysis when diagnostic testing is necessary in patients with possible acute gout.[45] Monosodium urate (MSU) crystals are visible in the joint aspirate from a gouty joint on polarised light microscopy.[45]
UK guidance states that a serum urate level of 360 micromol/L (6 mg/dL) or more confirms the diagnosis in those with signs and symptoms of gout.[31] If the serum urate level is below 360 micromol/L (6 mg/dL) during a flare and gout is strongly suspected, serum urate measurement should be repeated at least 2 weeks after the flare has settled.[31] Consideration should be given to joint aspiration and microscopy of synovial fluid if a diagnosis of gout remains uncertain or unconfirmed.[31]
The presence of calcium pyrophosphate dihydrate (CPPD) crystals in the joint aspirate (on polarised light microscopy) is the hallmark of pseudogout. Pseudogout can be accompanied by a number of co-morbid findings (e.g., haemochromatosis, hyperparathyroidism, hypomagnesaemia, hypophosphatasia, hypothyroidism, and familial hypocalciuric hypercalcaemia).[48][Figure caption and citation for the preceding image starts]: Calcium pyrophosphate dihydrate (CPPD) crystals in synovial fluid under compensated polarised light microscopyFrom the collection of Dr Soumya Chatterjee [Citation ends].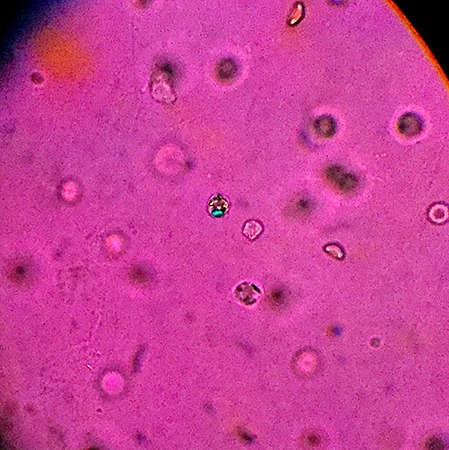
Reactive arthritis
Urine screening for C trachomatis is indicated in suspected cases of reactive arthritis with recent sexual activity and urethritis. Stool culture or serology for specific organisms should be guided by the clinical presentation and degree of suspicion. Note, however, that by the time arthritis develops, stool cultures are usually negative. Infections with Yersinia, Salmonella, Campylobacter, and Chlamydia cause strong antibody responses.
Lyme disease
Serological diagnosis for Lyme disease includes IgM and IgG antibodies via a 2-tier approach:[84][85][86] The first step should include a sensitive enzyme immunoassay (EIA) or immunofluorescence assay (IFA), and if positive or equivocal, this should be confirmed with a standardised Western blot assay. In the US, some EIAs have been approved by the US Food and Drug Administration for serological diagnosis of Lyme disease and can be used in place of Western blot assays for the second step.[84] For early Lyme disease (first 4 weeks), both IgM and IgG antibodies should be tested for in the second confirmatory step. No further testing is needed if specimens are negative by a sensitive EIA or IFA.
Indolent infections
Routine blood cultures and routine synovial fluid analysis, including cultures, are not useful in the diagnosis of indolent infections such as tuberculosis, brucellosis, or fungal infections. Specific synovial fluid studies (acid-fast bacilli, brucella, and fungal stains and special cultures) are required.
Anti-CCP antibodies are superior to RF in making the diagnosis of RA.[56]
Juvenile idiopathic arthritis
Children with systemic juvenile idiopathic arthritis (JIA) often have anaemia, thrombocytosis, and leukocytosis. ESR and CRP are elevated in different subtypes of the disease.
ANA is positive in oligo-articular JIA, and to a lesser extent in polyarticular JIA.
Systemic lupus erythematosus
The presence of ANA should be sought in cases suggestive of SLE, as it is positive in significant titre (usually 1:160 or higher) in nearly all patients with SLE. In addition to ANA, serology supporting a diagnosis of SLE includes positive anti-double stranded DNA and anti-Smith (Sm) antibodies.
Ankylosing spondylitis
HLA-B27 is present in 90-95% of white patients with AS.[87]
Enteropathic arthritides
For enteropathic arthritides, the following laboratory tests are helpful:
Faecal calprotectin: elevated levels are suggestive of inflammatory bowel disease. Confirmation of diagnosis requires colonic biopsy or small bowel biopsy.
Anti-transglutaminase, anti-endomysial, and anti-gliadin antibodies: coeliac disease is suggested by presence of these antibodies. Confirmation of diagnosis requires small bowel (duodenal) biopsy showing subtotal villous atrophy, and its reversibility with a gluten-free diet.
Tropheryma whipplei PCR on blood: suggestive of Whipple's disease, although the clinical use of this test has not yet been defined. Confirmation of diagnosis requires upper endoscopy with duodenal biopsy, and analysis of the specimen for periodic acid-Schiff (PAS) staining and PCR plus/minus immunohistochemistry staining forT whipplei. Fluid and/or tissue from synovium, cerebrospinal fluid, or affected lymph nodes may be used for the same tests.
Adult-onset Still’s disease
Serum ferritin is markedly elevated in adult-onset Still's disease (AOSD); the degree of elevation correlates with disease activity. The appearance of macrophage activation, in which the cells phagocytose haematopoietic elements, on bone marrow biopsy, can sometimes be seen (12% of patients).[72]
Acute rheumatic fever
There is no diagnostic laboratory test specific for ARF, and diagnosis is mostly based on high index of clinical suspicion. Throat cultures are negative in the majority of patients by the time ARF develops. If the antistreptolysin O (ASO) titre is negative, testing for other antistreptococcal antibodies, such as anti-DNAse B, antistreptokinase, and antihyaluronidase, should be performed.
Sarcoidosis
Very high serum ACE levels indicate the extent of granulomatous inflammation and may help to differentiate sarcoid from other causes of seronegative polyarthritis.
Parvovirus
Detectable levels of parvovirus B19-specific IgM can be found within 7 to 10 days of parvovirus exposure and remain measurable for several months.[88]
Arbovirus
The diagnosis of arbovirus infections (e.g., chikungunya) can be confirmed by viral culture, reverse transcription (RT)-PCR to detect viral RNA, or antibody tests including ELISA, immunofluorescence assays, and plaque-reduction neutralisation test.[89]
Imaging
X-rays of affected joints can provide useful clues regarding the nature of the joint problem.
X-ray following joint injury may reveal a fracture, a finding specifically sought whenever lipoid elements are present in the joint aspirate on microscopic examination.
In addition, typical changes can be seen in erosive arthritis, and characteristic features (peri-articular osteopenia, joint-space narrowing, new bone formation, bony ankylosis, calcinosis, chondrocalcinosis, or acro-osteolysis) can differentiate between RA, psoriatic arthritis, gout, pseudogout, haemochromatosis, hyperparathyroidism, scleroderma, osteoarthritis, erosive osteoarthritis, reflex sympathetic dystrophy, and multicentric reticulohistiocytosis.
DIP joint arthritis and arthritis mutilans (gross destruction of isolated joints; pencil-in-cup appearance) are typical radiographic findings for psoriatic arthritis. Other findings include acro-osteolysis, fluffy periostitis, and new bone formation at the site of enthesitis, joint lysis, and ankylosis.
In SAPHO syndrome, radiographs, isotope bone scans, and MRI scans may reveal evidence of sterno-clavicular joint arthritis, osteitis, and lytic, sclerotic, and hyperostotic bone lesions.
Cartilage loss in JIA presents as joint-space narrowing on joint x-ray, and, in long-standing disease, erosions are noted.
In RA, characteristic marginal erosions around MCP and PIP joints are often seen on x-ray or MRI scan. Subluxations and more severe joint damage are seen in advanced cases, but these findings are not specific.
Joint x-rays from patients with osteoarthritis show loss of joint space, subchondral sclerosis, cystic changes, and osteophytes. Typical central erosions, “gull-wing” and “saw-tooth” deformities, and ankylosis are seen in erosive osteoarthritis of fingers.
Half of patients with sarcoidosis present on chest x-ray with characteristic bilateral hilar lymph adenopathy, right paratracheal adenopathy, and pulmonary reticular opacities, usually in the upper zones. A PET scan may be helpful to identify the extent and distribution of occult sarcoid lesions.[90][Figure caption and citation for the preceding image starts]: Pulmonary sarcoidosis: right paratracheal, bilateral perihilar, and subcarinal adenopathyFrom the collection of Dr Soumya Chatterjee [Citation ends].
Musculoskeletal ultrasound is a very useful imaging modality that is non-invasive and radiation-free, and can be used at the bedside. It can be used both for diagnostic and therapeutic purposes (e.g., ultrasound-guided arthrocentesis, joint and soft-tissue injections). Musculoskeletal ultrasound has significantly improved diagnostic accuracy for a variety of rheumatological conditions. The American College of Rheumatology has published a report on reasonable use of musculoskeletal ultrasonography in rheumatology,[91] which discusses its use in the diagnosis of synovitis, synovial proliferation, bone erosions, joint effusion, tendinitis, tenosynovitis, enthesopathies, and crystal arthropathies (gout and calcium pyrophosphate arthropathy). Presence of large erosions in the second and fifth MCP, and the fifth MTP joints and distal ulna, are highly specific for and predictive of RA.[92] It has been shown that colour Doppler ultrasound is quite useful in distinguishing OA from inflammatory arthritis of the knee.[93] The recommendations of the European Society of Musculoskeletal Radiology also reinforce the use of this imaging modality.[94] On musculoskeletal ultrasound, the characteristic double contour sign helps establish a diagnosis of chronic gout.[95]
Dual-energy CT (DECT) scan has become an excellent non-invasive imaging modality for establishing a diagnosis of chronic gout, even during the intercritical periods.[95]
Biopsy
Synovial biopsy and culture may be necessary in the assessment and diagnosis of tuberculosis, and in non-tuberculous mycobacterial and fungal infections.
Biopsy and cytology may also be helpful in providing histological evidence of primary or metastatic intra-articular malignancy, synovial sarcoma, lipoma arborescens, and pigmented villonodular synovitis.
Sarcoid arthropathy may rarely require a synovial biopsy for diagnosis.
Confirmation of diagnosis of coeliac disease requires small bowel (duodenal) biopsy showing subtotal villous atrophy, and its reversibility with a gluten-free diet.
Confirmation of diagnosis of Whipple's disease requires upper endoscopy with duodenal biopsy, and analysis of the specimen for PAS staining and PCR and/or immunohistochemistry staining for T whipplei. Fluid and/or tissue from synovium, cerebrospinal fluid, or affected lymph nodes may be used for the same tests.
Use of this content is subject to our disclaimer