Investigations
1st investigations to order
non-contrast CT head
Test
Request brain imaging as soon as possible (at most within 1 hour of arrival at hospital).[68] Non-enhanced CT head is the investigation of choice in acute stroke.
Practical tip
Ring through to a radiologist on call to advise an immediate CT scan; speak to the radiographer to ensure the patient has the next available time slot.
Aim to take a collateral history from relatives regarding medications/past medical history while the patient is in the CT scanner.
Use the CT scan to differentiate between ischaemic stroke and haemorrhagic stroke; which must be done before starting thrombolysis in ischaemic stroke and before reversing anticoagulation in anticoagulation-induced intracerebral haemorrhage.[68][83]
Only healthcare professionals with appropriate training should interpret acute stroke imaging for thrombolysis or thrombectomy decisions.[83]
Remember that ischaemic stroke is a clinical diagnosis based on signs and symptoms; a normal CT scan does not rule out a stroke - particularly in the first few hours following a stroke, the CT scan can be normal or show very subtle ischaemic changes.
[Figure caption and citation for the preceding image starts]: Non-contrast CT scan of brain showing sub-acute isolated left basal ganglion infarction with left frontal horn mass effectCourtesy of BMJ Case Reports 2009; doi:10.1136/bcr.10.2008.1139 [Citation ends].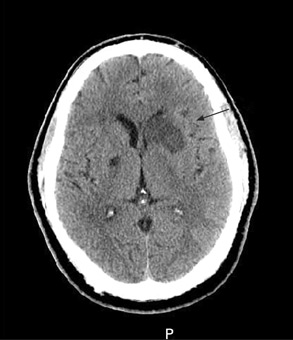
Result
hypoattenuation (darkness) of the brain parenchyma
loss of grey matter-white matter differentiation, and sulcal effacement
hyperattenuation (brightness) in an artery indicates clot within the vessel lumen
serum glucose
Test
Hypoglycaemia is a stroke mimic; hyperglycaemia has been associated with intracerebral bleeding and worse clinical outcomes in patients treated with intravenous thrombolysis.[67][69] You need to exclude both before giving thrombolysis.
Result
may be normal; may show hypoglycaemia or hyperglycaemia
serum electrolytes
Test
To exclude electrolyte disturbance (e.g., hyponatraemia) as a cause for sudden onset of neurological signs.
Result
may be normal; may show electrolyte disturbances
serum urea and creatinine
Test
To exclude renal failure because it may be a potential contraindication to some stroke interventions.
Result
may be normal; may show renal failure
cardiac enzymes
Test
To exclude concomitant myocardial infarction.
Result
may be normal; may show evidence of cardiac ischaemia
FBC
Test
To exclude anaemia or thrombocytopenia prior to possible initiation of thrombolysis, anticoagulants, or antithrombotics.
Result
may be normal; may show anaemia or thrombocytopenia
ECG
Test
To exclude cardiac arrhythmia (such as atrial fibrillation) or ischaemia, which are relatively common in ischaemic stroke.[80]
In people who would be eligible for secondary prevention treatment for atrial fibrillation or flutter:[68]
Perform prolonged ECG monitoring (at least 24 hours)
Consider prolonged sequential or continuous ECG monitoring with an external patch, wearable recorder, or implantable loop recorder in those in whom no other cause of stroke has been found, particularly if they have a pattern of cerebral ischaemia on brain imaging suggestive of cardioembolism.
Practical tip
Atrial fibrillation is a major preventable cause of ischaemic stroke.[29] Monitor all patients with suspected stroke for atrial fibrillation and other arrhythmias.[68] See New-onset atrial fibrillation.
The presence of paroxysmal atrial fibrillation has previously been underestimated, and latest guidance in the UK is to consider longer monitoring and implantable devices in more patients.[68][91]
Result
may be normal; may show arrhythmia or signs of ischaemia
prothrombin time and PTT (with INR)
Test
To exclude coagulopathy. Don’t delay thrombolysis (e.g., by waiting for test results) if the patient has no history of anticoagulant use, coagulopathy, or a condition that may lead to coagulopathy.[69]
Result
may be normal; may show coagulopathy
Investigations to consider
serum toxicology screen
Test
Consider a serum toxicology screen if you suspect ingestion of toxic substances. Signs and symptoms may mimic stroke.
Result
may exclude alcohol and drug ingestion
MRI head
Test
Consider diffusion-weighted MRI with stroke-specific sequences (diffusion-weighted imaging [DWI] with susceptibility weighted imaging [SWI] or T2*-weighted imaging) if the diagnosis remains uncertain despite CT.[68]
Practical tip
An MRI scan in the presence of ongoing symptoms is extremely likely to show the stroke. A normal MRI scan is very unlikely if the patient has had a stroke.[84]
[Figure caption and citation for the preceding image starts]: (A) Non-contrast T1-weighted MRI. (B) Post-contrast T1-weighted MRI showing minimal increase in leptomeningeal vessels over the right frontal region. (C) Diffusion-weighted image (DWI) showing a hyperintense area in the right frontal region. (D) Apparent diffusion coefficient (ADC) map shows hypointense lesion, indicating restricted diffusion that correlates with high intensity on DWI and exponential diffusion. (E) ADC value is 0.22 x 10³ mm²/second, corresponding to a hyperacute infarctFrom the personal collection of Eric E. Smith; used with permission [Citation ends].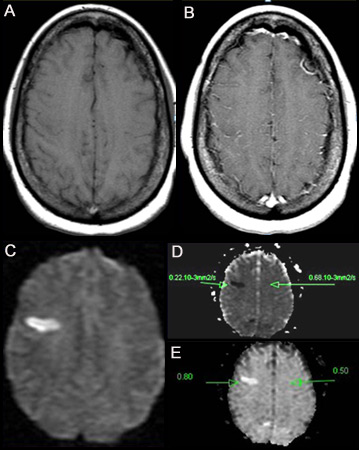
Result
acute ischaemic infarct appears bright on diffusion-weighted imaging
at later stages, T2 images may also show increased signal in the ischaemic territory
CT angiography
Test
Request a CT angiography (CTA) in patients with a suspected large vessel occlusion who are candidates for thrombectomy following the initial non-enhanced CT.[68]
Do not delay therapy with intravenous thrombolysis (if indicated) waiting to perform CTA or waiting for results.[70] In practice, hospitals that undertake CTA routinely in acute stroke give thrombolysis without waiting for the CTA report; they review the initial plain CT at the same time as performing the CTA.[70]
Use CTA preferentially over MRA because CTA gives quicker results.[67]
If the patient is a potential candidate for thrombectomy (i.e., onset of symptoms 6-24 hours) in addition to thrombolysis, request a CTA with contrast after (or with) the initial CT or MRI head to confirm occlusion of the proximal anterior circulation.[67]
Result
may be normal; may show arterial occlusion or stenosis
CT or MRI perfusion-weighted imaging
Test
Add CT perfusion imaging (or MR equivalent) if thrombectomy (at most within 1 hour of arrival at hospital) in patients with stroke with a delayed presentation for whom reperfusion is potentially indicated.[68] Studies have supported the use of perfusion scanning in patients to extend the thrombectomy window above 6 hours.[86][87][88]
UK guidelines recommend thrombectomy (± thrombolysis) for people who were last known to be well between 6 hours and 24 hours previously (including wake-up strokes) with confirmed occlusion of the proximal anterior or posterior circulation, if there is potential to salvage brain tissue as shown by perfusion imaging.[68]
[Figure caption and citation for the preceding image starts]: MRI arterial spin labelling image showing extensive hypoperfusion in the right cerebral hemisphere. There is a clear mismatch between diffusion and perfusionFrom the personal collection of Eric E. Smith; used with permission [Citation ends].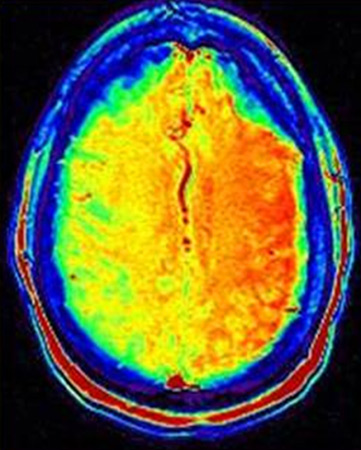
Result
shows areas with reduced blood flow that may be at risk for subsequent infarction
carotid ultrasound
Test
Patients with ischaemic stroke who after specialist assessment are considered candidates for carotid intervention should have carotid imaging performed within 24 hours of assessment. This includes carotid duplex ultrasound or either CT angiography or MR angiography.[68] Consult your local protocol on choice of investigation. Carotid duplex ultrasound is most commonly used.
Result
cervical artery occlusion or critical stenosis
echocardiogram
Test
If you suspect cardioaortic embolism, consider contrast transthoracic echocardiography (TTE) to evaluate the cardiac and aortic sources of embolus.[89] If no source is identified on TTE, use contrast transoesophageal echocardiography (TOE) in selected patients instead.[89]
Result
left atrial appendage thrombosis in patients with atrial fibrillation, valvular and prosthesis vegetations and thrombosis, aortic arch atheroma, patent foramen ovale, atrial septal defect, and intracardiac tumours
Use of this content is subject to our disclaimer