Investigations
1st investigations to order
blood cultures
Test
Blood cultures may be positive even if the pleural fluid culture is negative.
Should be taken before the initiation of antibiotics if the clinical state of the patient permits.
Result
positive for specific pathogens
CRP
Test
Part of a systemic response to infection.
Result
raised
WBC count
Test
Part of a systemic response to infection.
Result
raised
metabolic panel
Test
To include albumin and renal function tests. These help prognosticate patients that are at high risk for a poor outcome, using the RAPID (Renal [urea], Age, fluid Purulence, Infection source, Dietary [albumin]) clinical score.[25]
Result
varies
chest x-ray
Test
An urgent CXR should be scheduled in all patients who present with respiratory symptoms and evidence of sepsis.
Can demonstrate the presence of a pleural effusion.[8] A lateral decubitus CXR is more sensitive than a posteroanterior view for detecting an effusion, but its use has been superseded by thoracic ultrasound given the ease of rapid use and ubiquitous nature of ultrasound.
The presence of a loculated effusion suggests an empyema. Empyemas may have a pleurally based, 'D'-shaped appearance which can be mistaken for a lung mass.
In ventilated supine patients, a pleural effusion will appear as a diffuse unilateral increase in opacification.
There may be associated pulmonary consolidation due to pneumonia.
An effusion measuring >10 mm on a lateral decubitus CXR, in association with evidence of infection, requires thoracentesis (pleural aspiration).[1]
Result
blunting of costophrenic angle or effusion on affected side, possible consolidation, pleurally based 'D' shape in empyema
thoracic ultrasound
Test
More sensitive than a CXR for the detection of pleural effusions.[8]
Features suggestive of an empyema on ultrasound include the presence of echogenic fluid, loculations, and septations, as shown below.[28][Figure caption and citation for the preceding image starts]: Ultrasound image of heavily septated empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].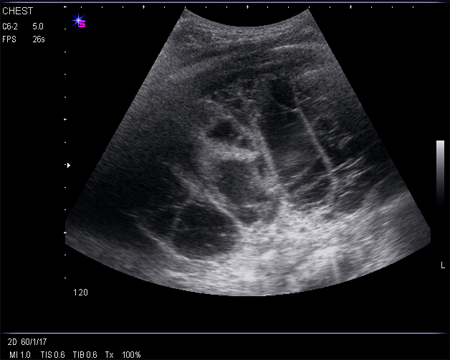
Empyemas are often associated with a raised haemidiaphragm or tethered lung; therefore, image guidance decreases complication rate substantially and so is preferred for all procedures.
The use of ultrasound to guide thoracentesis in order to reduce its associated complication rate is advised.[29]
Ultrasonography is also recommended to guide chest drain insertion, especially in small or loculated effusions.[8]
Result
presence of a pleural effusion which may be echogenic, loculated, and/or septated
thoracentesis: pleural fluid appearance
Test
Aspiration of frank pus is diagnostic of an empyema, and no other investigations are required to establish the diagnosis.
Result
frank pus in empyema, serous or cloudy in complicated parapneumonic effusions
thoracentesis: pleural fluid odour
Test
Putrid odour is suggestive of an anaerobic infection.
Result
putrid in anaerobic infection
thoracentesis: pleural fluid pH
Test
Samples should be stored anaerobically.[31] Local anaesthetics can falsely lower the pH. Physicians should have access to a blood gas analyser so that samples can be tested immediately to enable immediate insertion of a chest drain if indicated. If the sample is frank pus, the pH should not be tested as it can damage the analyser.
Result
<7.2
thoracentesis: pleural fluid total protein concentration
Test
If frank pus is aspirated, the protein concentration does not require analysis.
Result
>30 g/dL
thoracentesis: pleural fluid LDH level
Test
If frank pus is aspirated, the LDH level does not require analysis.
Result
>2-3 times above upper limit of normal range for serum
thoracentesis: pleural fluid glucose concentration
Test
If frank pus is aspirated, glucose does not require analysis. If an accurate pleural fluid pH is not available, low glucose levels can be used as an alternative predictor of a complicated parapneumonic effusion requiring urgent chest drain insertion. Pleural fluid glucose has been shown to be a robust predictor in this circumstance.[32]
Result
<3.3 mmol/L (60 mg/dL)
thoracentesis: pleural fluid white cell differential
Test
The predominance of lymphocytes in the exudate raises the suspicion of tuberculosis or malignancy.
Result
predominance of polymorphonuclear leukocytes (>90%)
thoracentesis: pleural fluid microscopy, culture, and sensitivity
Test
A positive Gram stain or culture is obtained in 60% to 70% of samples.[23] This can be used to guide antibiotic treatment.
Result
Gram-stain or culture positive
Investigations to consider
contrast-enhanced thoracic CT
Test
Chest CT should be reserved for complicated cases (e.g., children that fail to respond to treatment, or if there is doubt about the diagnosis).[26][27]
Done with tissue phase contrast. [Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of thoracic empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].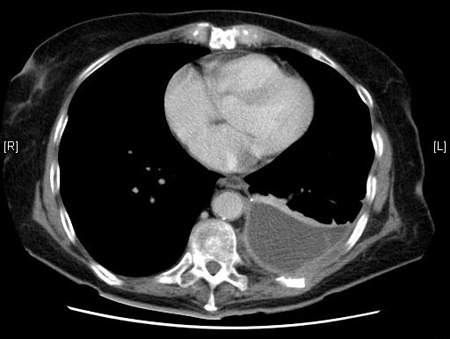
Can help distinguish empyema from other pleural effusions and lung abscesses.[33]
Enhancement of the pleura with contrast is characteristic of empyema.
Pleural thickening may be visible, but is also seen in malignancy.
The split pleura sign represents enhancement of the visceral and parietal pleura with interposed fluid.
Useful for confirmation of correct chest tube placement and to assess for source control and clearance of the pleural space. It may also help in the planning of surgery.
Result
lenticular pleural effusion causing compression of adjacent lung, 'split pleura sign', thickened pleura, loculations, septations, or gas bubbles, possible adjacent pneumonia
MRI of thorax
Test
An MRI is unable to accurately diagnose an empyema and is not routinely performed in the diagnosis or management of empyema. It is generally reserved for patients who are unable to undergo contrast-enhanced CT. It may show septations, loculated pleural fluid, or chest wall invasion.[34][Figure caption and citation for the preceding image starts]: MRI scan of septated empyemaFrom the collection of Najib Rahman, RTU, Oxford [Citation ends].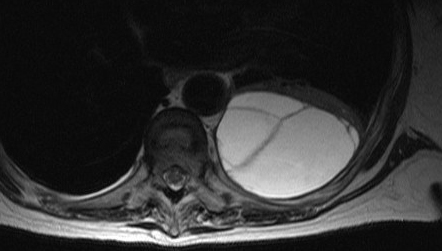
Result
septations, loculated pleural fluid, chest wall invasion
PET scan
Test
A PET scan is another possible imaging technique, but its use is limited by the fact that it is unable to distinguish between malignancy and empyema.[35] It is generally not performed in the diagnosis or management of empyema.
Result
fluorodeoxyglucose avid
pleural fluid polymerase chain reaction (PCR)
Test
As the causative organism in 40% of pleural infections remains unidentified, PCR may aid pathogen identification, allowing specific antibiotics to be chosen.[23]
Further prospective evidence is required on this technique.
Result
positive PCR for specific pathogens
Use of this content is subject to our disclaimer