Abstract
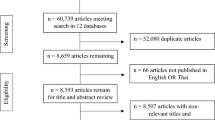
Despite recommendations in clinical practice guidelines, evidence suggests that utilization of cardiac rehabilitation (CR) following indicated cardiac events is low. Referral strategies, such as automatic referral, have been advocated to improve CR utilization. In this Review, we evaluate the effects of referral strategies on rates of CR referral and enrollment. Referral strategies are categorized as 'automatic' (the use of electronic health records or systematic discharge order sets), as 'liaison' (discussions with allied health-care providers), or as 'other' (for example, the use of motivational letter to patients). The highest rates of CR referral have been achieved in studies implementing automatic referral orders, whereas the highest rates of CR enrollment have resulted from a combination of automatic and liaison methods. Overall, innovative referral strategies significantly increase CR utilization. While further investigation is needed, institutions should evaluate their CR referral practice in light of these findings.
Key Points
-
Despite recommendations in clinical practice guidelines, evidence shows that only 15–20% of cardiac patients make use of cardiac rehabilitation services
-
The reasons for the disparity between evidence and care are complex but, arguably, the chief explanatory factors are referral failure and lack of provider encouragement
-
Innovative referral strategies can substantially increase cardiac rehabilitation referral and enrollment
-
Automatic referral methods, such as the AHA's Get With The Guidelines initiative, can appreciably increase referral rates
-
The incorporation of a cardiac rehabilitation referral discussion with an allied health-care provider can result in enrollment rates that are double the rates after usual referral
-
Innovative cardiac rehabilitation referral strategies should be considered by health-care providers, administrators and policy makers, although randomized trials are needed to clarify the role of each individual strategy
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Mackay, J. & Mensah, G. A. The Atlas of Heart Disease and Stroke [online], (WHO, Geneva, 2004).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet 364, 937–952 (2004).
Williams, M. A. Cardiovascular risk-factor reduction in elderly patients with cardiac disease. Phys. Ther. 76, 469–480 (1996).
Brown, A. et al. Exercise-based cardiac rehabilitation programs for coronary artery disease: a systematic clinical and economic review. Ottawa: Canadian Coordinating Office for Health Technology Assessment; 2003 Technology report no 34 [online], (2003).
Stone, J. A. et al. Canadian guidelines for cardiac rehabilitation and atherosclerotic heart disease prevention: a summary. Can. J. Cardiol. 17 (Suppl. B), 3B–30B (2001).
Thomas, R. J. et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, American College of Sports Medicine, American Physical Therapy Association, Canadian Association of Cardiac Rehabilitation, European Association for Cardiovascular Prevention and Rehabilitation, Inter-American Heart Foundation, National Association of Clinical Nurse Specialists, Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 50, 1400–1433 (2007).
Fischer, J. P. Automatic referral to cardiac rehabilitation. J. Cardiovasc. Nurs. 23, 474–479 (2008).
Centers for Medicare and Medicaid Services (CMS). Section 20.10: Cardiac rehabilitation programs in Medicare National Coverage Determinations Manual [online], (2008).
Taylor, R. S. et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am. J. Med. 116, 682–692 (2004).
Alter, D. A., Oh, P. I. & Chong, A. Relationship between cardiac rehabilitation and survival after acute cardiac hospitalization within a universal health care system. Eur. J. Cardiovasc. Prev. Rehabil. 16, 102–113 (2009).
Lavie, C. J. & Milani, R. V. Adverse psychological and coronary risk profiles in young patients with coronary artery disease and benefits of formal cardiac rehabilitation. Arch. Intern. Med. 166, 1878–1883 (2006).
Boulay, P. & Prud'homme, D. Health-care consumption and recurrent myocardial infarction after 1 year of conventional treatment versus short- and long-term cardiac rehabilitation. Prev. Med. 38, 586–593 (2004).
Digenio, A. G. & Joughin, H. M. Should all cardiac patients be offered the choice of cardiac rehabilitation? S. Afr. Med.J. 87 (Suppl. 3), C136–C144 (1997).
Papadakis, S. et al. Cost-effectiveness of cardiac rehabilitation program delivery models in patients at varying cardiac risk, reason for referral, and sex. Eur. J. Cardiovasc. Prev. Rehabil. 15, 347–353 (2008).
Canadian Association of Cardiac Rehabilitation. Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention: Translating Knowledge into Action, 3rd edn [online], (2009).
Graham, I. et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur. J. Cardiovasc. Prev. Rehabil. 14 (Suppl. 2), E1–E40 (2007).
Skinner, J. S., Cooper, A. & Feder, G. S. Secondary prevention for patients after a myocardial infarction: summary of NICE guidance. BMJ 334, 1112–1113 (2007).
Briffa, T. G. et al. Physical activity for people with cardiovascular disease: recommendations of the National Heart Foundation of Australia. Med. J. Aust. 184, 71–75 (2006).
The Australasian Society of Cardiac and Thoracic Surgeons and The Cardiac Society of Australia and New Zealand. National Heart Foundation Announcement. Heart Lung Circ. 13, 331–333 (2004).
Suaya, J. A. et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation 116, 1653–1662 (2007).
UK Department of Health. National service framework for coronary heart disease: modern tandards and service models [online], (2000).
Cortes, O. & Arthur, H. M. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am. Heart J. 151, 249–256 (2006).
Grace, S. L., Evindar, A., Abramson, B. L. & Stewart, D. E. Physician management preferences for cardiac patients: factors affecting referral to cardiac rehabilitation. Can. J. Cardiol. 20, 1101–1107 (2004).
Grace, S. L., Grewal, K. & Stewart, D. E. Differences in factors affecting cardiac rehabilitation referral by physician specialty. J. Cardiopulm. Rehabil. Prev. 28, 248–252 (2008).
Cohen, M. J., Pollak, A., Weiss, A. T. & Brezis, M. Availability bias in the management of myocardial infarction. QJM 99, 64–65 (2006).
Ades, P. A., Waldmann, M. L., McCann, W. J. & Weaver, S. O. Predictors of cardiac rehabilitation participation in older coronary patients. Arch. Intern. Med. 152, 1033–1035 (1992).
Cabana, M. D. et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 282, 1458–1465 (1999).
Witt, B. J., Thomas, R. J. & Roger, V. L. Cardiac rehabilitation after myocardial infarction: a review to understand barriers to participation and potential solutions. Eura. Medicophys. 41, 27–34 (2005).
Grace, S. L. et al. Contribution of patient and physician factors to cardiac rehabilitation enrollment: a prospective multi-level study. Eur. J. Cardiovasc. Prev. Rehabil. 15, 548–556 (2008).
Grace, S. L. et al. Contribution of patient and physician factors to cardiac rehabilitation referral: a prospective multi-level study. Nat. Clin. Pract. Cardiovasc. Med. 5, 653–662 (2008).
Grace, S. L. Barriers to cardiac rehabilitation referral. CICRP 13, 11–113 (2005).
Daly, J. et al. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog. Cardiovasc. Nurs. 17, 8–17 (2002).
Gurewich, D., Prottas, J., Bhalotra, S., Suaya, J. A. & Shepard, D. S. System-level factors and use of cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 28, 380–385 (2008).
Comoss, P. Improving utilization of cardiac rehabilitation services: where to start? J. Cardiovasc. Nurs. 23, 480–481 (2008).
Brown, T. M. et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: Results from the AHA's Get with the Guidelines program. Circulation 117, e465 (2008).
Williams, R. I., Fraser, A. G. & West, R. R. Gender differences in management after acute myocardial infarction: not 'sexism' but a reflection of age at presentation. J. Public Health (Oxf.) 26, 259–263 (2004).
Rhodes, R., Morrissey, M. J. & Ward, A. Self-motivation: a driving force for elders in cardiac rehabilitation. Geriatr. Nurs. 13, 94–98 (1992).
Pasquali, S. K., Alexander, K. P., Lytle, B. L., Coombs, L. P. & Peterson, E. D. Testing an intervention to increase cardiac rehabilitation enrollment after coronary artery bypass grafting. Am. J. Cardiol. 88, 1415–1416, A6 (2001).
Grace, S. L. et al. Cardiac rehabilitation II: referral and participation. Gen. Hosp. Psychiatry 24, 127–134 (2002).
Scott, L. B. Referral to outpatient cardiac rehabilitation: intervention research at the patient, provider, and health system levels. Nat. Clin. Pract. Cardiovasc. Med. 5, 671–672 (2008).
Cardiac Care Network of Ontario. The Ontario cardiac rehabilitation pilot project: report and recommendations [online], (2002).
Grace, S. L., Evindar, A., Kung, T. N., Scholey, P. E. & Stewart, D. E. Automatic referral to cardiac rehabilitation. Med. Care 42, 661–669 (2004).
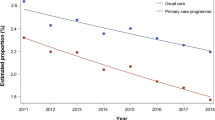
Grace, S. L. et al. A prospective comparison of cardiac rehabilitation enrollment following automatic vs usual referral. J. Rehabil. Med. 39, 239–245 (2007).
Grace, S. L. et al. Referral to and discharge from cardiac rehabilitation: key informant views on continuity of care. J. Eval. Clin. Pract. 12, 155–163 (2006).
Beswick, A. D. et al. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technol. Assess. 8, iii–iv, ix–x, 1–152 (2004).
Beswick, A. D. et al. Improving uptake and adherence in cardiac rehabilitation: literature review. J. Adv. Nurs. 49, 538–555 (2005).
American Heart Association. Get With The Guidelines [online], (2009).
Brown, T. M. et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: Results from the American Heart Association's Get With The Guidelines program. J. Am. Coll. Cardiol. 54, 515–521 (2009).
Grace, S. L., Evindar, A., Kung, T., Scholey, P. & Stewart, D. E. Increasing access to cardiac rehabilitation: automatic referral to the program nearest home. J. Cardiopulm. Rehabil. 24, 171–174 (2004).
LaBresh, K. A. et al. Improved treatment of hospitalized coronary artery disease patients with the Get With The Guidelines program. Crit. Pathw. Cardiol. 6, 98–105 (2007).
LaBresh, K. A., Ellrodt, A. G., Gliklich, R., Liljestrand, J. & Peto, R. Get With The Guidelines for cardiovascular secondary prevention: pilot results. Arch. Intern. Med. 164, 203–209 (2004).
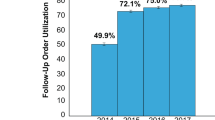
Mazzini, M. J., Stevens, G. R., Whalen, D., Ozonoff, A. & Balady, G. J. Effect of an American Heart Association Get With The Guidelines program-based clinical pathway on referral and enrollment into cardiac rehabilitation after acute myocardial infarction. Am. J. Cardiol. 101, 1084–1087 (2008).
Mosca, L., Han, R., Filip, J., McGillen, C. & Rubenfire, M. Barriers for physicians to refer to cardiac rehabilitation and impact of a critical care pathway on rates of participation [abstract]. Circulation 98 (Suppl. 17), I811 (1998).
Nori, D. et al. Use of discharge-worksheet enhances compliance with evidence-based myocardial infarction care. J. Thromb. Thrombolysis 14, 43–49 (2002).
Grace, S. L. et al. Potential of innovative cardiac rehabilitation techniques to increase utilization rates: preliminary results of the CRCARE study [abstract 0544]. Can. J. Cardiol. 24 (Suppl. SE) (2008).
Grace, S. L. et al. Increasing patient-initiation of cardiac rehabilitation referral in female percutaneous coronary intervention patients. Can. J. Cardiovasc. Nurs. 15, 23–27 (2005).
Carroll, D. L., Rankin, S. H. & Cooper, B. A. The effects of a collaborative peer advisor/advanced practice nurse intervention: cardiac rehabilitation participation and rehospitalization in older adults after a cardiac event. J. Cardiovasc. Nurs. 22, 313–319 (2007).
Jolly, K. et al. Randomised controlled trial of follow up care in general practice of patients with myocardial infarction and angina: final results of the Southampton Heart Integrated care Project (SHIP). BMJ 318, 706–711 (1999).
Leibowitz, M. et al. Coronary risk factor management in the framework of a community hospital-based ambulatory exercise training program. Prev. Cardiol. 7, 59–63 (2004).
Kalayi, C., Rimmer, F. & Maxwell, M. Improving referral for cardiac rehabilitation: an interface audit. J. Clin. Gov. 7, 143–145 (1999).
Mehta, R. H. et al. Quality improvement initiative and its impact on the management of patients with acute myocardial infarction. Arch. Intern. Med. 160, 3057–3062 (2000).
Harkness, K. et al. Effect of a postoperative telephone intervention on attendance at intake for cardiac rehabilitation after coronary artery bypass graft surgery. Heart Lung 34, 179–186 (2005).
Higgins, R. O. et al. Cardiac rehabilitation program attendance after coronary artery bypass surgery: overcoming the barriers. Med. J. Aust. 188, 712–714 (2008).
Suskin, N. et al. Improving cardiac rehabilitation (CR) participation in women and men, the CR participation study [abstract]. J. Cardiopulm. Rehabil. Prev. 27, 340–351 (2007).
Wyer, S. J. et al. Increasing attendance at a cardiac rehabilitation programme: an intervention study using the Theory of Planned Behaviour. Coron. Health Care 5, 154–159 (2001).
Smith, K. M. & Harkness, K. A. & Arthur, H. M. Predicting cardiac rehabilitation enrollment: the role of automatic physician referral. Eur. J. Cardiovasc. Prev. Rehabil. 13, 60–66 (2006).
Suskin, N. et al. Cardiac rehabilitation and secondary prevention services in Ontario: recommendations from a consensus panel. Can. J. Cardiol. 19, 833–838 (2003).
Goble, A. J. & Worcester, M. U. Heart Research Centre. Best practice guidelines for cardiac rehabilitation and secondary prevention. Department of Human Services Victoria [online], (1999).
Ajzen, I. in Action Control: From Cognition to Behavior (eds Kuhl, J. & Beckman, J.) 11–39 (Springer-Verlag, Berlin, 1985).
Kayaniyil, S., Leung, Y., Suskin, N., Stewart, D. E. & Grace, S. L. Concordance of self and program-reported rates of cardiac rehabilitation referral, enrollment and participation. Can. J. Cardiol. 25, e96–e99 (2009).
Everett, B., Salamonson, Y., Zecchin, R. & Davidson, P. M. Reframing the dilemma of poor attendance at cardiac rehabilitation: an exploration of ambivalence and the decisional balance. J. Clin. Nurs. 18, 1842–1849 (2009).
Grace, S. L., Suskin, N., Arthur, H. M. & Stewart, D. E. Automatic referral may reduce socioeconomic disparities in cardiac rehabilitation access. Presented at the 2007 National Health Care Leadership Conference.
Arthur, H. M. Improving secondary prevention of cardiovascular disease through referral to cardiac rehabilitation. JCOM 13, 572–577 (2006).
Taylor, R. S., Unal, B., Critchley, J. A. & Capewell, S. Mortality reductions in patients receiving exercise-based cardiac rehabilitation: how much can be attributed to cardiovascular risk factor improvements? Eur. J. Cardiovasc. Prev. Rehabil. 13, 369–374 (2006).
Dafoe, W., Arthur, H., Stokes, H., Morrin, L. & Beaton, L. for the Canadian Cardiovascular Society Access to Care Working Group on Cardiac Rehabilitation. Universal access: but when? Treating the right patient at the right time: access to cardiac rehabilitation. Can. J. Cardiol. 22, 905–911 (2006).
Tod, A. M., Lacey, E. A. & McNeill, F. 'I'm still waiting.': barriers to accessing cardiac rehabilitation services. J. Adv. Nurs. 40, 421–431 (2002).
Jolly, K. et al. The Birmingham Rehabilitation Uptake Maximisation study (BRUM): a randomised controlled trial comparing home-based with centre-based cardiac rehabilitation. Heart 95, 36–42 (2009).
Sparks, K. E., Shaw, D. K., Eddy, D., Hanigosky, P. & Vantrese, J. Alternatives for cardiac rehabilitation patients unable to return to a hospital-based program. Heart Lung 22, 298–303 (1993).
Dalal, H. M. et al. Home-based versus hospital-based rehabilitation after myocardial infarction: a randomized trial with preference arms—Cornwall Heart Attack Rehabilitation Management Study (CHARMS). Int. J. Cardiol. 119, 202–211 (2007).
Taylor, R. S. et al. Home-based cardiac rehabilitation versus hospital-based rehabilitation: a cost effectiveness analysis. Int. J. Cardiol. 119, 196–201 (2007).
British Heart Foundation. Cardiac rehabilitation—recovery or by-pass? National Campaign for Cardiac Rehabilitation [online], (2007).
Cardiac Health Foundation of Canada [online], (2009).
PCNA: Preventive Cardiovascular Nurses Association. J. Cardiovasc. Nurs. 21, 73–76 (2006).
Acknowledgements
This Review was supported by the Canadian Institutes of Health Research (CIHR) and The Heart and Stroke Foundation of Canada Grant # HOA-80676. S. Gravely-Witte is supported by an Ontario Women's Health Council/CIHR Institute of Gender and Health doctoral research award. Y. W. Leung is supported by a Canada Graduate Scholarship: Frederick Banting and Charles Best Canada doctoral award. S. L. Grace is supported by a CIHR New Investigator Award (# MSH-80489). We gratefully acknowledge Dr. Liane Ginsberg and Dr. Tamara Daly for their critiques on the proposal for this Review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Gravely-Witte, S., Leung, Y., Nariani, R. et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev Cardiol 7, 87–96 (2010). https://doi.org/10.1038/nrcardio.2009.223
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2009.223