Tests
1st tests to order
chest x-ray
Test
Should be obtained with any suspicion for HAP. Posterior-anterior and lateral views are preferred over anterior-posterior views. Comparison to an earlier film should be done if available.
All chest x-rays are limited by lack of differentiation between alveolar opacity and fluid.
A CT scan may be ordered to diagnose an opacity and clarify whether a procedure is indicated. [Figure caption and citation for the preceding image starts]: Portable chest x-ray of a patient with HAP. Note obscured left hemidiaphragm due to a left lower lobe opacity and an obscured heart border due to a left upper lobe or lingular opacityConsent obtained at University of Louisville, KY [Citation ends].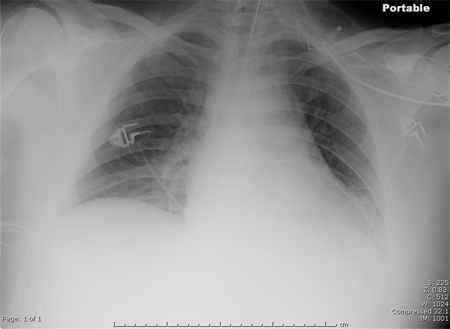
Result
opacity, blurring of diaphragm or heart border
WBC count with differential
Test
May be elevated with infection in general, but typically nonspecific. Bandemia is a concern above 4%, and leukopenia is a concern when there are less than 4000 cells/mL³.
Result
elevated or decreased WBC count above or below local laboratory normal values and/or elevated % bands
pulse oximetry
Test
Oxygen saturation measured by pulse oximetry can be deceivingly high compared with that obtained by an ABG.
Result
low value; <88% to <92% in general, but is relative to the baseline condition of the patient and supplemental oxygen
culture of lower respiratory tract sample
Test
A protected brush specimen (via bronchoscopy) has been regarded as the most accurate, followed by bronchoalveolar lavage, and tracheal aspirate through an endotracheal tube, but now noninvasive sampling (endotracheal aspiration) with semi-quantitative cultures is suggested as superior to invasive or noninvasive sampling with quantitative cultures.[1][58]
Positive cultures need to be correlated clinically, as they may merely be false positives showing evidence of colonization of the trachea or false negatives after prior antimicrobial treatment.
Quantitative cultures provide more information than qualitative specimens, and should be used if available.
Result
>10³ colony-forming units(cfu)/ mL for a protected brush specimen; >104 cfu/mL for bronchoalveolar lavage (BAL); >106 cfu/mL for endotracheal aspirate; 10⁴ or 10⁵ cfu/mL in the clinical context of ventilator-associated pneumonia
Tests to consider
ABG
Test
If HAP is suspected, the threshold to obtain an ABG should be low to ensure that the patient is not hypoxic.
Specific values cannot be given because all values of an ABG can be high or low based on a disease (such as HAP) and the degree of patient compensation.
Result
low pO₂; other ABG value abnormalities possible, such as values consistent with metabolic acidosis (e.g., low pH, high pCO₂)
diagnostic thoracentesis
Test
A thoracentesis should be performed if the amount of pleural fluid seen is considered to be more than minimal.[62]
Tests from pleural fluid that indicate that the pleural space needs to be drained are a pH <7.20, a glucose level <40 mg/dL, and an LDH level >1000 U/L.
Result
positive Gram stain or culture
CT chest
Test
A CT scan may be ordered to diagnose an opacity and clarify whether a procedure is indicated.[Figure caption and citation for the preceding image starts]: CT scan showing bibasilar opacities of patient with HAPConsent obtained at University of Louisville, KY [Citation ends].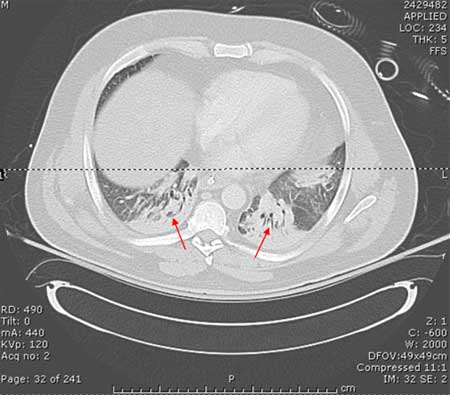 [Figure caption and citation for the preceding image starts]: CT scan of a patient with a large, dense left lower lobe infiltrateConsent obtained at University of Louisville, KY [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of a patient with a large, dense left lower lobe infiltrateConsent obtained at University of Louisville, KY [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan of a patient with a left lower lobe alveolar infiltrate (blue arrow), bilateral pleural effusions (yellow arrowheads), and right basilar atelectasis; notice the line separating the two shades of gray representing the infiltrate and the fluidConsent obtained at University of Louisville, KY [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan of a patient with a left lower lobe alveolar infiltrate (blue arrow), bilateral pleural effusions (yellow arrowheads), and right basilar atelectasis; notice the line separating the two shades of gray representing the infiltrate and the fluidConsent obtained at University of Louisville, KY [Citation ends].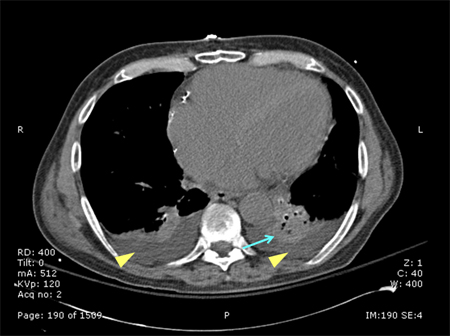
Result
may show an opacity or clarify findings if radiograph of poor quality
CRP
Test
The role of CRP is minimized in the 2016 Infectious Diseases Society of America and the American Thoracic Society guidelines for HAP/ventilator-associated pneumonia, where it is recommended that CRP does assist clinical exam when deciding to initiate antimicrobial therapy.[1]
Result
elevated
lung ultrasound
Emerging tests
MRSA nasal swab
Test
Nasal swabbing is increasingly being used to screen for MRSA in hospital settings. In the context of HAP/VAP, MRSA nasal swab screening can be used to guide de-escalation of empiric anti-MRSA therapy. In one meta-analysis of 22 studies, comprising 5163 participants, the specificity of MRSA nasal swabbing for MRSA VAP was 94%; the negative predictive value was 95%.[61] However, the Infectious Diseases Society of America guidelines do not include a recommendation on the use of nasal swabs to screen for MRSA in patients with HAP/VAP.[1]
Result
may be negative if no MRSA infection
Use of this content is subject to our disclaimer