Rib fractures
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
Look out for this icon: for treatment options that are affected, or added, as a result of your patient's comorbidities.
all patients
analgesia
Pain is imperative to treat as it improves pulmonary function and decreases the risk of pulmonary complications such as atelectasis, poor oxygenation, and respiratory compromise as well as reducing the risk of pneumonia, acute respiratory distress syndrome (ARDS), and respiratory failure.[27]Brasel KJ, Moore EE, Albrecht RA, et al. Western trauma association critical decisions in trauma: management of rib fractures. J Trauma Acute Care Surg. 2017 Jan;82(1):200-3. http://www.ncbi.nlm.nih.gov/pubmed/27779590?tool=bestpractice.com [45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf
Individualized multimodal analgesia based on age, level of pain, and extent of the injury is recommended for patients with multiple fractured ribs.[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf [46]Karmakar MK, Ho AM. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003 Mar;54(3):615-25. http://www.ncbi.nlm.nih.gov/pubmed/12634549?tool=bestpractice.com
Start scheduled analgesia as soon as possible with acetaminophen and a nonsteroidal anti-inflammatory drug (NSAID) such as ibuprofen (or, if regional block is likely to be needed, select a cyclo-oxygenase-2 [COX-2] inhibitor such as celecoxib to avoid platelet inhibition).[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf
Other analgesics that may be used include muscle relaxants (e.g., methocarbamol) and oral opioids (e.g., oxycodone), with escalation to intravenous opioids (e.g., morphine) and patient-controlled analgesia as needed (useful for breakthrough pain in particular).[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf Increased emphasis on nonopioid options such as NSAIDs, acetaminophen, gabapentin, lidocaine topical patches, and methocarbamol (i.e., “multimodal analgesia”) may reduce opioid use.[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf [47]Burton SW, Riojas C, Gesin G, et al. Multimodal analgesia reduces opioid requirements in trauma patients with rib fractures. J Trauma Acute Care Surg. 2022 Mar 1;92(3):588-96. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8866226 http://www.ncbi.nlm.nih.gov/pubmed/34882599?tool=bestpractice.com [48]Martin TJ, Eltorai AS, Dunn R, et al. Clinical management of rib fractures and methods for prevention of pulmonary complications: a review. Injury. 2019 Jun;50(6):1159-65. http://www.ncbi.nlm.nih.gov/pubmed/31047683?tool=bestpractice.com
A range of analgesia may be used for patients with complicated, multiple, or bilateral rib fractures, including regional nerve blocks (e.g., serratus anterior, paravertebral or intercostal blocks) or thoracic epidural anesthesia.[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf There are many options for regional anesthesia, which can be tailored to the patient. Early use of regional anesthesia can avoid the potential complications associated with opioid use.[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf Epidural analgesia improved pain relief compared with other analgesic interventions in one meta-analysis.[27]Brasel KJ, Moore EE, Albrecht RA, et al. Western trauma association critical decisions in trauma: management of rib fractures. J Trauma Acute Care Surg. 2017 Jan;82(1):200-3. http://www.ncbi.nlm.nih.gov/pubmed/27779590?tool=bestpractice.com [49]Peek J, Smeeing DPJ, Hietbrink F, et al. Comparison of analgesic interventions for traumatic rib fractures: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2018 Feb 6;45(4):597-622. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6689037 http://www.ncbi.nlm.nih.gov/pubmed/29411048?tool=bestpractice.com
However further meta-analyses variously report that, compared with other analgesic modalities, epidural anesthesia does not reduce mortality, ICU or hospital length of stay, length of mechanical ventilation, or pulmonary complications in patients with multiple traumatic rib fractures.[49]Peek J, Smeeing DPJ, Hietbrink F, et al. Comparison of analgesic interventions for traumatic rib fractures: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2018 Feb 6;45(4):597-622. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6689037 http://www.ncbi.nlm.nih.gov/pubmed/29411048?tool=bestpractice.com [50]Carrier FM, Turgeon AF, Nicole PC, et al. Effect of epidural analgesia in patients with traumatic rib fractures: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth. 2009 Mar;56(3):230-42. http://www.ncbi.nlm.nih.gov/pubmed/19247744?tool=bestpractice.com A lidocaine topical patch can be an alternative to regional anesthesia.[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf [51]Cheng YJ. Lidocaine skin patch (Lidopat® 5%) is effective in the treatment of traumatic rib fractures: a prospective double-blinded and vehicle-controlled study. Med Princ Pract. 2016;25(1):36-9. https://pmc.ncbi.nlm.nih.gov/articles/PMC5588305 http://www.ncbi.nlm.nih.gov/pubmed/26539836?tool=bestpractice.com [52]Johnson M, Strait L, Ata A, et al. Do lidocaine patches reduce opioid use in acute rib fractures? Am Surg. 2020 Sep;86(9):1153-8. http://www.ncbi.nlm.nih.gov/pubmed/32812770?tool=bestpractice.com
Also consider nonpharmacologic alternatives, particularly for uncomplicated rib fractures (e.g., positioning, transcutaneous electrical stimulation, and ice).[45]American College of Surgeons. Best practices guideline for acute pain management in trauma patients. Nov 2020 [internet publication]. https://www.facs.org/media/exob3dwk/acute_pain_guidelines.pdf [53]Oncel M, Sencan S, Yildiz H, et al. Transcutaneous electrical nerve stimulation for pain management in patients with uncomplicated minor rib fractures. Eur J Cardiothorac Surg. 2002 Jul;22(1):13-7. http://ejcts.oxfordjournals.org/content/22/1/13.long http://www.ncbi.nlm.nih.gov/pubmed/12103366?tool=bestpractice.com [54]Hsu JR, Mir H, Wally MK, et al. Clinical practice guidelines for pain management in acute musculoskeletal injury. J Orthop Trauma. 2019 May;33(5):e158-82. https://pmc.ncbi.nlm.nih.gov/articles/PMC6485308 http://www.ncbi.nlm.nih.gov/pubmed/30681429?tool=bestpractice.com
Stress fractures, which often occur in athletes, are initially treated with periods of rest, analgesia, and activity modification until symptoms resolve.[44]Reeder MT, Dick BH, Atkins JK, et al. Stress fractures: current concepts of diagnosis and treatment. Sports Med. 1996 Sep;22(3):198-212. http://www.ncbi.nlm.nih.gov/pubmed/8883216?tool=bestpractice.com
Primary options
acetaminophen: children <12 years of age: 10-15 mg/kg orally every 4-6 hours when required, maximum 75 mg/kg/day; children ≥12 years of age: 325-650 mg orally every 4-6 hours when required, maximum 4000 mg/day; adults: 325-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
-- AND --
ibuprofen: children ≥6 months of age: 5-10 mg/kg orally every 6-8 hours when required, maximum 40 mg/kg/day; children ≥12 years of age and adults: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day (children) or 3200 mg/day (adults)
or
celecoxib: adults: 100-200 mg orally twice daily
OR
lidocaine topical patch: adults: dose depends on brand of transdermal patch; consult product literature for guidance on dose
OR
gabapentin: adults: 300 mg orally once daily on day 1, followed by 300 mg twice daily on day 2, then 300 mg three times daily, increase gradually according to response, maximum 3600 mg/day
OR
methocarbamol: adults: 1500 mg orally four times daily for 2-3 days, followed by 1000 mg four times daily or 1500 mg three times daily or 750 mg every 4 hours, maximum 8000 mg/day (initial starting dose) or 4500 mg/day (subsequent dose)
Secondary options
oxycodone: children: consult specialist for guidance on dose; adults: 5-15 mg orally (immediate-release) every 4-6 hours when required, adjust dose according to response
Tertiary options
morphine sulfate: children: consult specialist for guidance on dose; adults: 2.5 to 10 mg subcutaneously/intravenously/intramuscularly every 2-6 hours when required, adjust dose according to response
These drug options and doses relate to a patient with no comorbidities.
Primary options
acetaminophen: children <12 years of age: 10-15 mg/kg orally every 4-6 hours when required, maximum 75 mg/kg/day; children ≥12 years of age: 325-650 mg orally every 4-6 hours when required, maximum 4000 mg/day; adults: 325-1000 mg orally every 4-6 hours when required, maximum 4000 mg/day
-- AND --
ibuprofen: children ≥6 months of age: 5-10 mg/kg orally every 6-8 hours when required, maximum 40 mg/kg/day; children ≥12 years of age and adults: 400 mg orally every 4-6 hours when required, maximum 2400 mg/day (children) or 3200 mg/day (adults)
or
celecoxib: adults: 100-200 mg orally twice daily
OR
lidocaine topical patch: adults: dose depends on brand of transdermal patch; consult product literature for guidance on dose
OR
gabapentin: adults: 300 mg orally once daily on day 1, followed by 300 mg twice daily on day 2, then 300 mg three times daily, increase gradually according to response, maximum 3600 mg/day
OR
methocarbamol: adults: 1500 mg orally four times daily for 2-3 days, followed by 1000 mg four times daily or 1500 mg three times daily or 750 mg every 4 hours, maximum 8000 mg/day (initial starting dose) or 4500 mg/day (subsequent dose)
Secondary options
oxycodone: children: consult specialist for guidance on dose; adults: 5-15 mg orally (immediate-release) every 4-6 hours when required, adjust dose according to response
Tertiary options
morphine sulfate: children: consult specialist for guidance on dose; adults: 2.5 to 10 mg subcutaneously/intravenously/intramuscularly every 2-6 hours when required, adjust dose according to response
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
acetaminophen
-- AND --
ibuprofen
or
celecoxib
OR
lidocaine topical patch
OR
gabapentin
OR
methocarbamol
Secondary options
oxycodone
Tertiary options
morphine sulfate
respiratory physical therapy
Treatment recommended for ALL patients in selected patient group
Rib fractures impair adequate ventilation resulting in atelectasis, poor oxygenation, and respiratory compromise.[27]Brasel KJ, Moore EE, Albrecht RA, et al. Western trauma association critical decisions in trauma: management of rib fractures. J Trauma Acute Care Surg. 2017 Jan;82(1):200-3. http://www.ncbi.nlm.nih.gov/pubmed/27779590?tool=bestpractice.com Early chest physical therapy and mobility are emphasized to improve pulmonary toilet (mucus and secretion clearance techniques). Breathing exercises assessed with incentive spirometry and assisted coughing may help prevent complications.[42]Battle C, Pelo C, Hsu J, et al. Expert consensus guidance on respiratory physiotherapy and rehabilitation of patients with rib fractures: an international, multidisciplinary e-Delphi study. J Trauma Acute Care Surg. 2023 Apr 1;94(4):578-83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10045972 http://www.ncbi.nlm.nih.gov/pubmed/36728349?tool=bestpractice.com [56]Mukherjee K, Schubl SD, Tominaga G, et al. Non-surgical management and analgesia strategies for older adults with multiple rib fractures: a systematic review, meta-analysis, and joint practice management guideline from the Eastern Association for the Surgery of Trauma and the Chest Wall Injury Society. J Trauma Acute Care Surg. 2023 Mar 1;94(3):398-407. http://www.ncbi.nlm.nih.gov/pubmed/36730672?tool=bestpractice.com
oxygen
Treatment recommended for SOME patients in selected patient group
Administer oxygen as indicated to treat hypoxia.[55]Williams A, Bigham C, Marchbank A. Anaesthetic and surgical management of rib fractures. BJA Educ. 2020 Oct;20(10):332-40. https://pmc.ncbi.nlm.nih.gov/articles/PMC7807920 http://www.ncbi.nlm.nih.gov/pubmed/33456914?tool=bestpractice.com Impaired oxygenation can occur due to impaired effort of ventilation with chest wall pain or be indicative of underlying pneumothorax, hemothorax, or pulmonary contusion.[27]Brasel KJ, Moore EE, Albrecht RA, et al. Western trauma association critical decisions in trauma: management of rib fractures. J Trauma Acute Care Surg. 2017 Jan;82(1):200-3. http://www.ncbi.nlm.nih.gov/pubmed/27779590?tool=bestpractice.com
treatment of underlying cause
Treatment recommended for SOME patients in selected patient group
If the patient has a prior history of malignancy, metastatic disease should be suspected. Metastasis from lung, prostate, breast, and liver cancer can involve the ribs, accounting for 12.6% of metastatic lesions.[15]Xu DL, Zhang XT, Wang GH, et al. Clinical features of pathologically confirmed metastatic bone tumors: a report of 390 cases [in Chinese]. Ai Zheng. 2005 Nov;24(11):1404-7. http://www.ncbi.nlm.nih.gov/pubmed/16552972?tool=bestpractice.com There are numerous primary bone tumors that can present as pathologic rib fractures, including osteochondroma, enchondroma, plasmacytoma, chondrosarcoma, and osteosarcoma; about 37% of lesions are malignant.[16]Aydoğdu K, Findik G, Agackiran Y, et al. Primary tumors of the ribs; experience with 78 patients. Interact Cardiovasc Thorac Surg. 2009 Aug;9(2):251-4. https://academic.oup.com/icvts/article/9/2/251/729805 http://www.ncbi.nlm.nih.gov/pubmed/19447801?tool=bestpractice.com These should be managed with appropriate specialist referral and treatment.
As age increases, the absolute risk of sustaining a fragility fracture is inversely proportional to the patient's bone mineral density, with about 27% of these fractures occurring in the ribs.[4]Siris ES, Brenneman SK, Barrett-Connor E, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006;17(4):565-74. http://www.ncbi.nlm.nih.gov/pubmed/16392027?tool=bestpractice.com Therefore, osteoporosis should be treated.
In children, the presence of rib fractures without associated trauma has the highest probability of being attributed to physical abuse when compared with all other fractures.[14]Kemp AM, Dunstan F, Harrison S, et al. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008 Oct 2;337:a1518. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563260/?tool=pubmed http://www.ncbi.nlm.nih.gov/pubmed/18832412?tool=bestpractice.com Among infants younger than 12 months presenting with rib fractures, as many as 82% sustained these injuries through physical abuse.[2]Bulloch B, Schubert CJ, Brophy PD, et al. Cause and clinical characteristics of rib fractures in infants. Pediatrics. 2000 Apr;105(4):E48. http://pediatrics.aappublications.org/content/105/4/e48.full http://www.ncbi.nlm.nih.gov/pubmed/10742369?tool=bestpractice.com [3]Paine CW, Fakeye O, Christian CW, et al. Prevalence of Abuse Among Young Children With Rib Fractures: A Systematic Review. Pediatr Emerg Care. 2019 Feb;35(2):96-103. http://www.ncbi.nlm.nih.gov/pubmed/27749806?tool=bestpractice.com A consultation with child protective services should be considered in all children with suspected physical abuse.
management of complications
Treatment recommended for ALL patients in selected patient group
Pneumothorax occurs in about 14% to 37% of rib fractures, hemopneumothorax in 20% to 27%, pulmonary contusions in 17%, and a flail chest in up to 6%.[8]Sirmali M, Türüt H, Topçu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003 Jul;24(1):133-8. https://academic.oup.com/ejcts/article/24/1/133/375481 http://www.ncbi.nlm.nih.gov/pubmed/12853057?tool=bestpractice.com [9]Keel M, Meier C. Chest injuries - what is new? Curr Opin Crit Care. 2007 Dec;13(6):674-9. http://www.ncbi.nlm.nih.gov/pubmed/17975389?tool=bestpractice.com [10]Liman ST, Kuzucu A, Tastepe AI, et al. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003 Mar;23(3):374-8. http://ejcts.oxfordjournals.org/content/23/3/374.long http://www.ncbi.nlm.nih.gov/pubmed/12614809?tool=bestpractice.com Traumatic injuries to the first rib have a 3% risk of concomitant great vessel injury.[23]Gupta A, Jamshidi M, Rubin JR. Traumatic first rib fracture: is angiography necessary? A review of 730 cases. Cardiovasc Surg. 1997 Feb;5(1):48-53. http://www.ncbi.nlm.nih.gov/pubmed/9158123?tool=bestpractice.com
A tube thoracostomy may be necessary to either decompress a pneumothorax or drain the hemothorax. See Pneumothorax.[Figure caption and citation for the preceding image starts]: CT scan showing large left-sided pneumothoraxFrom the collection of Dr Paul Novakovich; used with permission [Citation ends].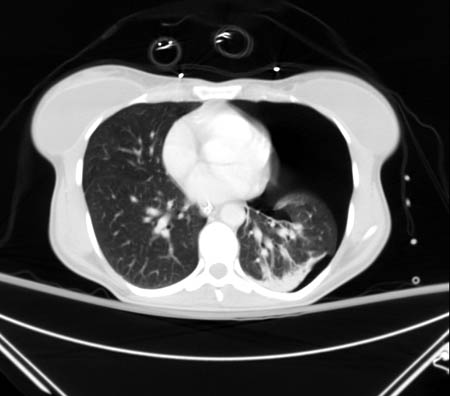 [Figure caption and citation for the preceding image starts]: CXR depicting the same pneumothorax as shown on CTFrom the collection of Dr Paul Novakovich; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: CXR depicting the same pneumothorax as shown on CTFrom the collection of Dr Paul Novakovich; used with permission [Citation ends].
Because of the multitude of associated injuries, the treating physician should have a high suspicion for closed-head injuries, solid organ injuries, spine injuries, and extremity fractures. Consultation with the appropriate service should not be delayed if any associated injury is encountered.
How to insert an intercostal (chest) drain using the open technique. Video demonstrates: tube selection, how to identify the site for drain insertion, how to make the correct incision, how to insert the intercostal drain, how to secure the drain, and postprocedure care.
mechanical ventilation
Treatment recommended for SOME patients in selected patient group
Mechanical ventilation may be necessary for unstable patients.[56]Mukherjee K, Schubl SD, Tominaga G, et al. Non-surgical management and analgesia strategies for older adults with multiple rib fractures: a systematic review, meta-analysis, and joint practice management guideline from the Eastern Association for the Surgery of Trauma and the Chest Wall Injury Society. J Trauma Acute Care Surg. 2023 Mar 1;94(3):398-407. http://www.ncbi.nlm.nih.gov/pubmed/36730672?tool=bestpractice.com
Isolated rib fractures rarely require mechanical ventilation unless associated with other injuries, such as pulmonary contusion.[60]Chest trauma. In: Hess DR, Kacmarek RM, eds. Essentials of mechanical ventilation. 3rd ed. New York: McGraw-Hill Education; 2014.
For patients with flail chest mechanical ventilation is only needed if they present with shock, a head injury, severe pulmonary dysfunction, a deteriorating respiratory status, or if immediate surgery is required.[60]Chest trauma. In: Hess DR, Kacmarek RM, eds. Essentials of mechanical ventilation. 3rd ed. New York: McGraw-Hill Education; 2014.
Internal fixation of ribs/flail chest may be considered where there is difficulty weaning the patient from mechanical ventilation, or when thoracotomy is required for other reasons.[61]Simon B, Ebert J, Bokhari F, et al; Eastern Association for the Surgery of Trauma. Management of pulmonary contusion and flail chest: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012 Nov;73(5 Suppl 4):S351-61. https://www.east.org/education/practice-management-guidelines http://www.ncbi.nlm.nih.gov/pubmed/23114493?tool=bestpractice.com [62]Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013 Dec;258(6):914-21. http://www.ncbi.nlm.nih.gov/pubmed/23511840?tool=bestpractice.com [63]Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013 May;216(5):924-32. http://www.ncbi.nlm.nih.gov/pubmed/23415550?tool=bestpractice.com
Systematic reviews have reported an association between operative management of rib fractures in flail chest and reduced ventilator requirements, as well as earlier discharge from intensive care.[62]Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013 Dec;258(6):914-21. http://www.ncbi.nlm.nih.gov/pubmed/23511840?tool=bestpractice.com [63]Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013 May;216(5):924-32. http://www.ncbi.nlm.nih.gov/pubmed/23415550?tool=bestpractice.com [64]Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017 Mar;82(3):618-26. https://journals.lww.com/jtrauma/Fulltext/2017/03000/Operative_fixation_of_rib_fractures_after_blunt.25.aspx http://www.ncbi.nlm.nih.gov/pubmed/28030502?tool=bestpractice.com [65]Schuurmans J, Goslings JC, Schepers T. Operative management versus non-operative management of rib fractures in flail chest injuries: a systematic review. Eur J Trauma Emerg Surg. 2017 Apr;43(2):163-8. https://pmc.ncbi.nlm.nih.gov/articles/PMC5378742 http://www.ncbi.nlm.nih.gov/pubmed/27572897?tool=bestpractice.com This effect may be less pronounced in the presence of pulmonary contusion.[62]Leinicke JA, Elmore L, Freeman BD, et al. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013 Dec;258(6):914-21. http://www.ncbi.nlm.nih.gov/pubmed/23511840?tool=bestpractice.com
surgical stabilization
Treatment recommended for SOME patients in selected patient group
Surgical stabilization of rib fractures may be considered in patients with flail chest, patients with multiple severely displaced rib fractures, or patients who fail to respond to optimal nonoperative management.[66]Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury. 2017 Feb;48(2):307-21. http://www.ncbi.nlm.nih.gov/pubmed/27912931?tool=bestpractice.com
Operative treatment of rib fractures in flail chest is associated with reductions in: the number of days spent on mechanical ventilation; hospital and intensive care length of stay; the rate of pneumonia; the need for tracheostomy; the degree of chest wall deformity; and the cost of treatment.[64]Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017 Mar;82(3):618-26. https://journals.lww.com/jtrauma/Fulltext/2017/03000/Operative_fixation_of_rib_fractures_after_blunt.25.aspx http://www.ncbi.nlm.nih.gov/pubmed/28030502?tool=bestpractice.com [67]Lucena-Amaro S, Cole E, Zolfaghari P. Long term outcomes following rib fracture fixation in patients with major chest trauma. Injury. 2022 Sep;53(9):2947-52. http://www.ncbi.nlm.nih.gov/pubmed/35513938?tool=bestpractice.com [69]Wang Z, Jia Y, Li M. The effectiveness of early surgical stabilization for multiple rib fractures: a multicenter randomized controlled trial. J Cardiothorac Surg. 2023 Apr 10;18(1):118. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10084648 http://www.ncbi.nlm.nih.gov/pubmed/37038166?tool=bestpractice.com However, any effect on mortality remains uncertain.[64]Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017 Mar;82(3):618-26. https://journals.lww.com/jtrauma/Fulltext/2017/03000/Operative_fixation_of_rib_fractures_after_blunt.25.aspx http://www.ncbi.nlm.nih.gov/pubmed/28030502?tool=bestpractice.com In addition, the quality of the evidence upon which these recommendations are based is relatively poor.[66]Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury. 2017 Feb;48(2):307-21. http://www.ncbi.nlm.nih.gov/pubmed/27912931?tool=bestpractice.com
While surgical stabilization of fractures is now included within standard treatment, it is not widely practiced and requires ongoing trials in expert centers.

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer

