History and exam
Key diagnostic factors
common
blood at one nostril or on both sides of nose
Blood is usually found in one nostril or on both sides of the nose by the time a patient presents with active epistaxis.
presence of risk factors
Risk factors for epistaxis are many and varied. They include:
Age:
Epistaxis is more common in children and older people.[10]
Environmental:
Cold, dry, low humidity weather, or marked variations in air temperature and pressure.[16]
Local nasal:
Minor trauma, such as nose picking or rubbing[10]
Rubbing, sneezing, coughing, or straining can precipitate epistaxis in children
Recent upper respiratory tract infection, rhinitis, or rhinosinusitis causing mucosal friability
Corticosteroid nasal spray causing friable nasal mucosa[16][17]
Drug misuse (particularly cocaine)[10]
Foreign body (particularly relevant to children).[10]
In practice, a unilateral foul-smelling nasal discharge is a more common presentation than epistaxis.
Increased risk of bleeding:
Comorbidities that may affect the patient’s response to a bleed or indicate that they may be on antithrombotic therapy:
Other diagnostic factors
common
bleeding starting at the nares
Suggests an anterior site for the source of bleeding.
Anterior epistaxis quickly causes blood in the pharynx, so identifying whether a bleed started in the front of the nose or down the throat is helpful.
Anterior epistaxis will present in the throat, however, if originating while the patient is supine.
recurrent epistaxis
Recurrent significant nosebleed suggests anterior vessel on affected side.
Common in children.[10]
septal deviation
May increase likelihood for epistaxis.[10]
uncommon
bleeding starting in the throat
Suggests a posterior site as the source of bleeding.
Anterior epistaxis will present in the throat, however, if originating while the patient is supine.
signs of haemodynamic compromise
intranasal polyp
A cause of recurrent epistaxis
Rare in children.
telangiectasia
Hereditary haemorrhagic telangiectasia (HHT) is an autosomal dominant genetic disease leading to arteriovenous malformations and telangiectasias.[10]
Causes recurrent epistaxis in >90% of people with hereditary haemorrhagic telangiectasia.[10]
Associated with:[10]
Multiple telangiectasias of the face, lips, oral cavity, nasal cavity, and/or fingers
Arteriovenous malformations in the lungs, liver, gastrointestinal tract, or brain
Presence in a first-degree relative.
[Figure caption and citation for the preceding image starts]: Multiple telangiectasias visible on nasal examinationImage used with permission from BMJ 2019;367:l5393 doi: 10.1136/bmj.l5393 [Citation ends].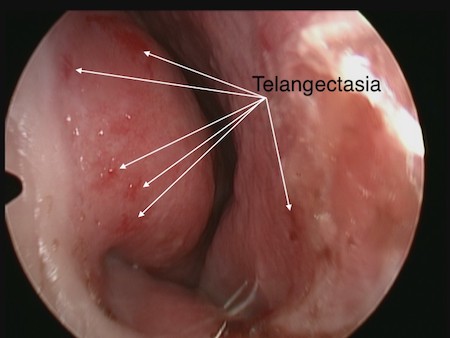
Use of this content is subject to our disclaimer