Recommendations
Urgent
Use the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach.[44]
Consider putting out a trauma call if the patient is unstable or has multiple injuries. Have a low threshold in patients with facial injuries, suspected head injury, or rib fractures, particularly if anticoagulated.
Provide analgesia immediately and reassess after 30 minutes. Use your hospital’s prescribing protocol, or National Institute for Health and Care Excellence (NICE) recommendations:[45]
Give paracetamol preoperatively if not contraindicated
Add an opioid if paracetamol and the block (if used) are not sufficient
Older people may need reduced doses of opioids. Start on the lowest possible dose and titrate up as necessary
Give orally if possible
Offer paracetamol with or without an opioid postoperatively
Avoid non-steroidal anti-inflammatory drugs as these can be associated with serious adverse effects
Consider arranging a femoral nerve block or fascia iliaca compartment block by a trained practitioner.[45][54]
Request an orthopaedic opinion urgently.
Guidelines recommend surgery on the day of, or the day after, admission to avoid increased risk of mortality.[45][46][47]
Assess fluid status and resuscitate with intravenous fluids.[46]
Key Recommendations
Initial treatment
Older patients should have multidisciplinary care on an orthogeriatric ward to reduce the risk of complications after surgery for hip fracture.[45] These include delirium.
Ensure there is assessment by a senior orthogeriatrician as soon as possible and within 72 hours.[46][47]
Continue to assess pain hourly until the patient is settled on a ward, and regularly thereafter.[45]
Provide analgesia to patients with cognitive impairment even if not reporting pain.
Ensure thorough clerking including comorbidities, medication, and functional status to guide management plan.
Review medication
Consider essential medications that should be continued
Consider reversal of anticoagulation
Consider withholding medications that may cause perioperative hypotension or acute kidney injury.
Assess the patient’s nutritional status within the first 24 hours of admission.[46] Prescribe dietary supplements for those who are malnourished or at risk.
Presurgical assessment
Arrange a group and save and crossmatch if the patient is likely to require blood transfusion.
Assess the patient’s bleeding and venous thromboembolism risk prior to surgery.[76]
Administer prophylactic antibiotics.[77][78]
Usually at induction of anaesthesia.
Base the choice of drug on your local antibiotic prescribing protocol.
Discuss and document ceilings of care.
Involve the patient and any family members or carers in these discussions, as appropriate.
Consider any advanced directives, lasting powers of attorney, and safeguarding issues.[79]
Risk stratification
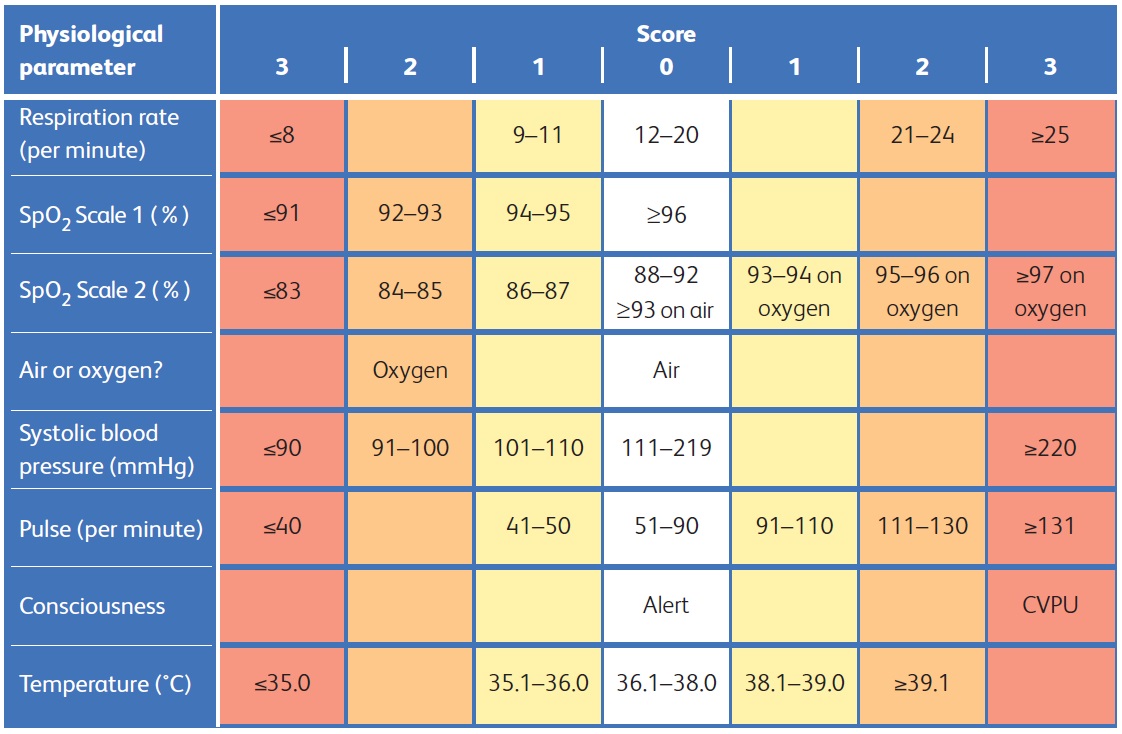
Assess any immediate risk to the patient using an early warning score such as the National Early Warning Score (NEWS2).[66] Use a mortality risk score, such as the Nottingham Hip Fracture Score, or the American Society of Anesthesiologists physical status classification system, to plan care and to communicate risk with patients and carers.[80][81]
Assess mental state
Use a standardised and validated measure.[51][52] Use the 4AT assessment for delirium.[52] In critical care or in the recovery room after surgery, use the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) or Intensive Care Delirium Screening Checklist (ICDSC) instead of the 4AT.[52]
Surgery
Surgery must be carried out on the day of, or the day after, admission to avoid increased risk of mortality.[45][46][47]
Choice of procedure depends on the location of the fracture, the degree of displacement, and the presence or absence of instability.
If currently unsuitable for surgery, reassess daily for sufficient improvement to reconsider surgery.
Postoperative care
Review the patient’s analgesia and other medications.
There may be routine medications that you can now reintroduce.
Review the wound and the patient’s bowel and bladder function.
Rehabilitation and discharge planning
Review estimated discharge date daily with the multidisciplinary team. Aim for rehabilitation in the patient’s usual place of residence where possible.[46]
Liaise with or follow up on falls assessment, physiotherapy, and occupational therapy to understand the patient’s functional status and care needs and impact on discharge planning.
Discharge patients with severe frailty with appropriate care and provide an advanced care plan as soon as possible.
The main treatment goals are to:
Relieve pain
Restore mobility
Manage any intercurrent illness
Prevent further falls and fractures.
Manage the patient using the ABCDE approach.[44]
Ensure the patient is stable.
Consider putting out a trauma call if needed.
If the patient is older and/or frail, involve the multidisciplinary team. Ideally treat the patient on an orthogeriatric ward to reduce the risk of complications, such as delirium, as per guidelines from NICE, the British Orthopaedic Association Standards for Trauma and Orthopaedics (BOAST), and the National Hip Fracture Database.[45][47][82]
Obtain an orthopaedic opinion urgently.
Treat any acute concurrent medical illness, such as sepsis, as this may affect the patient’s suitability for surgery.
If currently unsuitable for surgery, reassess daily for sufficient improvement to reconsider surgery.
Assess fluid status and resuscitate with intravenous fluids as appropriate.[46]
Patients usually need fluid resuscitation and maintenance fluids preoperatively.
Blood loss, pain, confusion, and fasting for theatre (the operating room) all contribute to a reduced oral intake throughout admission.[46]
Older patients with frailty may not exhibit the usual signs of dehydration, such as tachycardia or hypotension.[46]
Ensure thorough clerking including comorbidities, medication, and functional status to guide management plan.
Assess the patient’s nutritional status within the first 24 hours of admission.[46] Prescribe dietary supplements for those who are malnourished or at risk.
Ensure there is assessment by a senior orthogeriatrician as soon as possible and within 72 hours.[46][47]
This should include:
Documentation of pre-existing frailty
Assessment for delirium and dementia
Assessment and treatment of existing medical conditions
Comprehensive falls assessment
An assessment of bone health
Estimation of discharge date in line with the multidisciplinary team.
Manage the patient in a frailty pathway that includes Comprehensive Geriatric Assessment (to determine the medical, psychological, and functional capability of an older patient with frailty) starting within 72 hours of injury.[79]
Consider essential medications that should be continued and consider reversal of anticoagulation. Consider withholding medications that may cause perioperative hypotension or acute kidney injury.
Continue to monitor for other injuries associated with any trauma requiring urgent treatment.
Review the pressure area assessment and protect any vulnerable skin areas to prevent incipient pressure ulcers.
The pressure area assessment should be completed by nursing staff on admission.
Patients with hip fractures are at high risk of developing pressure sores.[46]
Provide the patient and carer with verbal and printed information about diagnosis, choice of anaesthesia, and surgical procedures.
Involve an orthogeriatrician or perioperative physician in optimising the patient for surgery and agreeing appropriate ceilings of care with the patient, relatives, and team.
Liaise with the anaesthetist and high-dependency unit/intensive care unit where necessary.
Arrange a falls assessment (if not already arranged as part of the orthogeriatric assessment) as the patient is likely to be at risk of further falls during admission.[46]
All patients with hip fractures must have a falls risk assessment on admission as part of the nursing assessment and a care plan to modify risk factors put in place (e.g., sensors on the bed).[46]
The patient should be assessed by a physiotherapist on the day of or the day after surgery.[46][47][79]
Liaise with occupational therapy to understand the patient’s functional status and care needs and impact on discharge planning.
An occupational therapist assessment should occur early after admission to understand the patient’s functional baseline care need provision, and expectations about discharge.[46]
Treat the patient's pain immediately, even before investigations, and reassess pain relief after 30 minutes.[45] Continue to assess pain hourly until the patient is settled on the ward, and then regularly thereafter.[45]
Use a pain assessment score.
Use your hospital’s analgesic prescribing protocol, or NICE recommendations:[45]
Give paracetamol preoperatively if not contraindicated.
Add an opioid if paracetamol and the block (if used) are not sufficient. Older people may need reduced doses of opioids. Start on the lowest possible dose and titrate up as necessary. Give orally if possible.
Offer paracetamol with or without an opioid postoperatively.
Do not use non-steroidal anti-inflammatory drugs due to their adverse effects, such as upper gastrointestinal bleeding, nephrotoxicity, and fluid retention. Older people are more susceptible to these effects.
Consider arranging a femoral nerve block or fascia iliaca compartment block by a trained practitioner.[45][54]
Ensure there is sufficient analgesia for any investigations.
Nerve blocks
Nerve blocks (i.e., femoral nerve block or fascia iliaca compartment block) are effective in relieving pain and can reduce the need for opioids.[59][83] This is important in older patients who are often more sensitive to the adverse effects of opioids, such as constipation, delirium, and nausea.[54]
The procedures should be carried out only by someone with prior training. They may be performed with ultrasound guidance.
The block may be repeated by the anaesthetic team, to provide initial postoperative pain relief (i.e., for the first postoperative night).[59]
Nerve blocks may reduce the time to first mobilisation after the surgical procedure (but the evidence for this is less clear).[83]
Complications of a fascia iliaca compartment block are rare, but include:[84]
Local anaesthetic toxicity
The risk of this is highest in the first 15 to 30 minutes, so the patient must be closely monitored at this stage
Signs include perioral numbness, tinnitus, dizziness, arrhythmia, seizures
Intravascular injection
Temporary or permanent nerve damage
Infection
Block failure
Injury secondary to numbness/weakness of limb
Allergy.
Encourage intake of oral fluids up to 2 hours prior to surgery. This prevents dehydration and improves the patient’s comfort.[46] Avoid repeatedly fasting patients in preparation for surgery.[46]
The orthopaedic surgeon will consent the patient, mark the limb, and confirm the likely timing of surgery so the nil-by-mouth policy can be initiated.
Prior to surgery, identify and treat any correctable comorbidities so that surgery is not delayed.[45] These may include:
Anaemia
Consider the cause of anaemia and whether it is acute or chronic. If the fracture is unexplained, consider a diagnosis of myeloma and offer a full blood count and blood tests for calcium and plasma viscosity or erythrocyte sedimentation rate.[49]
Follow local protocols for when a preoperative blood transfusion is necessary.
Ensure appropriate investigations including haematinics are sent prior to transfusion.
Consider early discussion with a haematologist if macrocytic anaemia is present.
A haemoglobin concentration <80 g/L (<8 g/dL) may be a reason to delay surgery.[59]
Uncontrolled diabetes
Review local guidelines for management.
Monitor blood sugars perioperatively.
Anticoagulation
Attend to a reversible coagulopathy so that it does not cause an unnecessary delay to surgery.[59]
Consider the indication for the oral anticoagulant and, if high risk, whether bridging anticoagulation (using a short-acting parenteral anticoagulant while the oral anticoagulant is temporarily stopped) is required.
Consider the timing of the last dose, the half-life of the drug, and whether it will require active reversal for surgery and anaesthetic (also need to know when surgery is planned).
Volume depletion
Electrolyte imbalance
Arrhythmia
Perform an ECG preoperatively to enable cardiac assessment.
Assess for common medical conditions, such as decompensated heart failure, poorly controlled atrial fibrillation, and exacerbation of chronic obstructive airways disease.
Manage as per local guidelines.
Consider an urgent medical review if the patient is unstable.
Provide patients and carers with verbal and written information about anaesthetic and surgical choices and the likelihood of a functional recovery.
Practical tip
It is essential to have a multidisciplinary approach to presurgical assessment. Decisions regarding risks and benefits to delaying surgery are best made with senior nursing, orthopaedic, anaesthetic, and orthogeriatric involvement. Involve patients and their families in discussions and decisions.
Thromboprophylaxis
Assess the patient’s bleeding and venous thromboembolism risk prior to surgery.[76][79]
Total hip arthroplasty, open reduction and internal fixation of hip fractures, and surgery due to major trauma are among the orthopaedic procedures with the highest deep vein thrombosis risk.[85] The prevalence of venous thromboembolism after total hip arthroplasty has been reported to be up to 22% even with the use of pharmacological prophylaxis.[85][86]
NICE recommends the Department of Health venous thromboembolism risk assessment tool.[76] Department of Health VTE risk assessment tool Opens in new window
Reassess the risk of bleeding and venous thromboembolism at the point of consultant review or if the patient’s clinical condition changes.
Arrange a group and save and crossmatch.
Factors that may indicate a higher risk of bleeding include:[87]
Trochanteric fracture
Initial haemoglobin level <120 g/L (<12 g/dL)
Age older than 75 years.
For patients on an anticoagulant, send a coagulation screen and follow local guidelines to correct any coagulopathy. Follow your hospital protocol for patients taking a direct oral anticoagulant (DOAC) or discuss with a haematologist.
Venous thromboembolism prophylaxis with either a low molecular weight heparin (LMWH) or fondaparinux may be needed for people who are immobile and whose risk of venous thromboembolism outweighs their risk of bleeding.[76]
Consider preoperative venous thromboembolism prophylaxis for people with fragility fractures of the pelvis, hip, or proximal femur if surgery is delayed beyond the day after admission.[76]
Give the last dose no less than 12 hours before surgery for LMWH, or 24 hours before surgery for fondaparinux.
Offer venous thromboembolism prophylaxis for 1 month after surgery to people with fragility fractures (i.e., a fracture sustained from a fall from a standing height) of the pelvis, hip, or proximal femur if the risk of venous thromboembolism outweighs the risk of bleeding.[76]
Choose either:[76]
LMWH starting 6 to 12 hours after surgery
Fondaparinux starting 6 hours after surgery (providing there is a low risk of bleeding based on their bleeding risk assessment).
Consider stopping prophylaxis if lower limb immobilisation continues beyond 42 days.[76]
If pharmacological prophylaxis is contraindicated, consider intermittent pneumatic compression for people with fragility fractures of the pelvis, hip, or proximal femur at the time of admission. Continue until mobility is restored to the patient’s baseline level.[76]
Compression stockings may cause severe discomfort and worsen skin conditions.
Antibiotic prophylaxis
Give a single intravenous dose of a suitable prophylactic antibiotic (e.g., ceftriaxone) on induction of anaesthesia.[77][78]
Use your local antibiotic prescribing protocol.
Identify patients at risk of infection with MRSA, such as MRSA carriers.
A nasal swab should be performed by nursing staff on admission.
Give appropriate prophylaxis, which will depend on the resistance profile.
Seek specialist advice from a microbiologist.
Tranexamic acid
Consider tranexamic acid.
There is evidence to support the use of tranexamic acid to reduce blood loss and blood transfusion in patients with hip fracture.[88][89][90]
Multidisciplinary teams should agree local policies on the use of tranexamic acid in this setting.[91]
Traction
Do not routinely use preoperative traction as it is not effective in relieving pain or easing reduction during surgery.
There may be advantages for specific fracture types, but there is no evidence to confirm this.[92]
Ceilings of care
Discuss and document ceilings of care. Involve the patient and any family members or carers in these discussions, as appropriate.
Consider any advanced directives, lasting powers of attorney, and safeguarding issues.[79]
Make an immediate assessment of the patient using an early warning score, such as the NEWS2 score, and follow up using a scoring system at least every 12 hours.[46][66] Assess:
Respiration rate
Oxygen saturation
Systolic blood pressure
Pulse rate
Level of consciousness or new-onset confusion
Temperature
Allocate a score from 0 to 3 to each parameter as they are measured. The magnitude of the score reflects how much the parameter varies from the norm. The score is aggregated and uplifted by 2 points for people requiring supplemental oxygen to maintain their recommended oxygen saturation.[66] [Figure caption and citation for the preceding image starts]: National Early Warning Score 2 (NEWS2) is an early warning score produced by the Royal College of Physicians in the UK. It is based on the assessment of six individual parameters, which are assigned a score of between 0 and 3: respiratory rate, oxygen saturations, temperature, blood pressure, heart rate, and level of consciousness. There are different scales for oxygen saturation levels based on a patient’s physiological target (with scale 2 being used for patients at risk of hypercapnic respiratory failure). The score is then aggregated to give a final total score; the higher the score, the higher the risk of clinical deteriorationReproduced from: Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: RCP, 2017. [Citation ends].
Practical tip
Consider the NEWS score in the context of the patient’s comorbidities: for example, confusion may be due to existing dementia, or low oxygen saturations may be due to COPD.
Use a mortality risk score, such as the Nottingham Hip Fracture Score, or the American Society of Anesthesiologists (ASA) physical status classification system, to plan care and to communicate risk with patients and carers. [80][81]
The ASA classification system grades a patient's health and comorbidities before an operative procedure, and has been shown to predict outcome.[81]
The Nottingham Hip Fracture Score is a specific predictor of 30-day mortality after hip fracture repair.
It assigns a numerical score to seven preoperative variables: age, sex, admission haemoglobin, mini mental test score 6 or lower out of 10, patient living in an institution, two or more comorbidities, and presence of malignancy.[93]
Evidence: Risk of mortality
Mortality risk varies between patient populations. Patient characteristics may be identified on admission to predict mortality risk.
A systematic review and meta-analysis of 53 studies including 544,733 participants identified the following statistically significant pre-admission characteristics, which predicted a greater risk of mortality at 12 months following hip fracture:[94]
Male sex
Age ≥85 years
Care homes resident
Presence of an intracapsular fracture
Requires assistance to mobilise
Cognitive impairment
Abnormal ECG on admission
Poor general health.
The four characteristics indicating the highest risk of mortality at 12 months were:[94]
Reduced pre-fracture mobility
Age >85 years
Abnormal ECG
Cognitive impairment.
Use a standardised and validated measure to check for cognitive impairment.[51][52]
Use the 4AT assessment for delirium. In critical care or in the recovery room after surgery, use the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) or Intensive Care Delirium Screening Checklist (ICDSC) instead of the 4AT.[52]
Between 35% and 65% of older patients with hip fracture will develop delirium in hospital.[46]
Delirium increases length of hospital stay and hospital-associated adverse events, such as falls.
Delirium is often under-diagnosed.[46]
Signs of delirium include:[52]
Confusion and disorientation
Visual or auditory hallucinations
Restlessness
Agitation
Changes in appetite
Sleep disturbance
Lack of co-operation with reasonable requests
Withdrawal
Changes in communication, mood, and/or attitude.
Explain about risk of delirium postoperatively and encourage unrestricted visiting immediately postoperatively.
If you suspect delirium, request an orthogeriatric opinion.
Use the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) or Intensive Care Delirium Screening Checklist (ICDSC) score after surgery.[52]
Guidelines recommend surgery on the day of, or the day after, admission to avoid increased risk of mortality.[45][46][47]
Early surgery:
Allows earlier mobilisation and functional recovery
Is associated with less pain and reduced length of hospital stay.[95]
Evidence: Timing of surgery
Perform surgery on the day of, or the day after, admission to avoid increased risk of mortality and complications.
Delayed fixation of a hip fracture is associated with increased 1-year mortality, increased complications, and increased hospital stay.[46] Therefore, older patients with frailty and with multiple comorbidities must be rapidly assessed and optimised for surgery without causing any delay.
NICE states that early and appropriate surgery is the most effective form of pain relief, expediting rehabilitation and reducing complications.
Postponement of surgery carries an increased risk of complications, as well as prolongation of pain, and the need for repeated preoperative fasting.[45]
A delay of 24 to 36 hours allows these factors to be balanced with appropriate assessment and allows patients to be operated on in a planned trauma list.
A systematic review and meta-analysis looked at 16 prospective or retrospective observational studies (involving 257,367 patients) on surgical timing and mortality in hip fracture.[96]
It found that operative delay beyond 48 hours after admission may increase the odds of 30-day all-cause mortality by 41% and of 1-year all-cause mortality by 32%.
Another study on whether the timing of surgery in such patients could influence the short-term clinical outcome looked at 36-hour and 48-hour time limits.[97]
Patients who had the operation more than 36 and 48 hours after admission were less likely to return to independent living within 4 months (odds ratio 0.44 and 0.33, respectively), whereas there was no significant difference with use of the 24-hour cut-off limit.
The incidence of pressure ulcers in the groups that had the operation later was increased at all three cut-off limits (a delay of more than 24 hours, more than 36 hours, and more than 48 hours) (odds ratio 2.19, 3.42, and 4.34, respectively).
The length of hospitalisation was also increased in the groups that had the later operation (median of 14 compared with 18 days, 15 compared with 19 days, and 15 compared with 21 days, respectively) (P <0.001 for all comparisons).
The risks and benefits of spinal or general anaesthesia should be discussed with the patient preoperatively.[45]
The estimated blood loss associated with different surgical procedures will vary. Transfusion to prevent unacceptable postoperative anaemia may be necessary.
The patient should be able to fully bear weight on the affected limb in the immediate postoperative period.[45]
Check operation note for any restrictions.
Operative management results in a reduced length of hospital stay and improved rehabilitation compared with conservative methods (bed rest and traction), which are no longer recommended.[98]
Perform all necessary safety checks to confirm the procedure, site, and side of the surgery.[99]
Follow safety procedures on prosthesis verification.[99]
Choice of procedure
Choice of procedure depends on the location of the fracture and whether it is displaced.
Intracapsular fracture
An intracapsular hip fracture may be undisplaced or displaced.
Undisplaced:
Displaced, or undisplaced but not suitable for fixation:
Offer replacement arthroplasty ( total hip replacement or hemiarthroplasty)[45][59]
Offer total hip replacement rather than hemiarthroplasty to patients who:[45]
Were able to walk independently out of doors with no more than the use of a stick, AND
Do not have a condition or comorbidity that makes the procedure unsuitable for them, AND
Are expected to be able to carry out activities of daily living independently beyond 2 years.
A minority of patients may have displaced intracapsular fractures that will be fixed or reduced and fixed rather than treated with arthroplasty: for example, young patients, and some valgus impacted fractures.
For patients with valgus impacted fractures, also consider non-operative management on a case-by-case basis.
Extracapsular fracture
For patients with an extracapsular hip fracture:[45][59]
Use a dynamic hip screw for fixation of stable intertrochanteric hip fractures
Use an intramedullary nail to treat patients with subtrochanteric fractures.
Pathological fracture
Manage patients with a pathological fracture due to bony metastases in conjunction with an oncology/regional bone tumour service.[9] The surgical procedure required is likely to be different.
Evidence: Choice of procedure
Choice of procedure depends on the location of the fracture and whether it is displaced.
A Cochrane review comparing the relative effects (benefits and harms) of any type of internal fixation versus any type of arthroplasty for intracapsular hip fractures in adults looked at the results of 19 trials.[101]
Length of surgery, operative blood loss, need for blood transfusion, and risk of deep wound infection were significantly less for internal fixation compared with arthroplasty.
Fixation had a significantly higher re-operation rate compared with arthroplasty (40% versus 11%; risk ratio 3.22, 95% CI 2.31 to 4.47, 19 trials).
No definite differences for hospital stay, mortality, or regain of pre-injury residential state were found.
NICE recommends:[45]
Replacement arthroplasty (total or hemiarthroplasty) for patients with a displaced intracapsular hip fracture
A sliding hip screw in preference to an intramedullary nail in patients with trochanteric fractures above and including the lesser trochanter
An intramedullary nail to treat a subtrochanteric fracture.
Non-surgical interventions include analgesia and bed rest/non-weight bearing. The outcomes for these patients are poor.
Only consider non-surgical interventions for:
Patients who are at the end stage of a terminal illness (i.e., where life expectancy is less than 72 hours)[53]
Non-ambulatory patients where pain is well controlled on toileting and for nursing care.
Patients with valgus impacted intracapsular fractures who are able to mobilise without significant pain.
There is a risk that non-operative management in this group will fail and that the fracture may become displaced, or that the patient develops avascular necrosis requiring later surgery.
Identify and treat any contributory causes to the fracture.
Consider:
What caused the fall?
This may be factors such as:
Cognitive impairment (confusion, delirium, dementia)
Poor vision
Balance or mobility problems
Frailty
Hazardous environment
Collapse due to a medical reason (e.g., arrhythmia, transient ischaemic attack, hypoglycaemia).
What caused the bone to fracture?
This may include:
Osteoporosis
Vitamin D deficiency
Malignancy.
Every patient should have a physiotherapy assessment as soon as possible.
Mobilise the patient on the day of or the day after surgery.[45][46][47]
Aim to have patients standing, using equipment where necessary.
Patients who cannot stand should be hoisted out to a chair.
Occupational therapy assessment is needed by the end of the third postoperative day.[46]
Consider dietician review in patients who are malnourished or at risk of malnourishment.
Assess the patient’s bone health to prevent future fractures. The patient is now at higher risk of another fracture and risk factors should be reduced if possible.[46]
A previous fracture will approximately double the risk of a subsequent fracture, with the greatest risk occurring in the first year following the incident fracture.[46]
A meta-analysis of previous fracture and subsequent fracture risk showed that previous fracture history was associated with a significantly increased risk of any fracture compared with individuals without a prior fracture (RR 1.86, 95% CI 1.75 to 1.98). The risk ratio was similar for the outcome of osteoporotic fracture and for hip fracture. There was no significant difference in risk ratio between men and women.[102]
Continue to evaluate pain and give regular analgesia.[45] Postoperative analgesia requirements will vary considerably.[59]
Review the wound.
Check for signs of infection.
Liaise with nursing staff.
Review bladder and bowels.
Prescribe to prevent constipation as needed.
Remove urinary catheters.
Practical tip
In patients with a high risk of urinary retention (history of prostate disease or spinal stenosis) it may be more successful to remove the catheter once the patient can stand.
Give verbal and written information on the signs and symptoms of deep vein thrombosis and pulmonary embolism, how patients can reduce their risk, and how to seek help if these are suspected.
Test for delirium within the week after surgery.[47]
Delirium is the most common complication of all forms of surgery and anaesthesia in older people.[47] Use the 4AT assessment for delirium.[52]
With senior colleagues and your multidisciplinary team, consider end-of-life care as necessary.
Falls risk assessment
Identify patients with frailty as ‘at risk of falls using tools such as the electronic frailty index (eFI) and ensure appropriate follow-up is given.[51]
Perform a multifactorial falls risk assessment prior to discharge. This includes:[42]
Identification of falls history
Assessment of gait, balance and mobility, and muscle weakness
Assessment of osteoporosis risk
Assessment of the older person's perceived functional ability and fear relating to falling
Assessment of visual impairment
Assessment of cognitive impairment and neurological examination
Assessment of urinary incontinence
Assessment of home hazards
Cardiovascular examination
Medication review.
Address future falls risk and offer an individualised intervention aimed at promoting independence and improving physical and psychological function.
These assessments and interventions are likely to be offered by the multidisciplinary team (orthogeriatrician, nurses, physiotherapists, occupational therapists).
Offer physiotherapy and multidisciplinary rehabilitation programmes to restore patients to pre-fracture functioning with the aim of returning them to where they lived pre-fracture.[103][104]
Offer access to interventions and services that reduce falls and fracture risk factors such as:[51]
Strength and balance training. A meta-analysis of 40 randomised controlled trials (n=4059) showed that interventions targeting improvement in mobility after hip fracture may cause clinically meaningful improvement in mobility and walking speed in hospital and post‐hospital settings, compared with conventional care. Interventions that include gait and balance training and functional tasks are particularly effective.[105]
Smoking cessation.
Reducing alcohol intake.
Follow-up
Follow up patients who have had a total hip replacement or intramedullary nailing (until satisfactory union occurs).
Review estimated discharge date daily with the multidisciplinary team.
Aim to return patients to their original residence after their surgery, ideally within 30 days, and offer 120-day follow-up as recommended in the National Hip Fracture Database report.[45][46][47]
Coordinated multidisciplinary rehabilitation programmes may result in an increased percentage of patients returning home and remaining there following a hip fracture.[103][104][106]
More than 10% of patients will be unable to return to their previous residence. Most will have some residual pain or disability.[1]
Set reasonable expectations for recovery. Some loss of function is to be expected in most patients.[1]
Patients may require long-term care or aides for walking.
Use of this content is subject to our disclaimer