Investigations
1st investigations to order
ECG
Test
Record and interpret a resting 12-lead ECG within 10 minutes of the point of first medical contact in any patient with suspected cardiac chest pain.[7]
Discuss the patient immediately with the cardiology team and involve senior support if the ECG shows evidence of ST-elevation myocardial infarction (STEMI) to activate your local STEMI protocol.[7] See ST-elevation myocardial infarction.
Abnormal findings that suggest NSTEMI include:[1][7]
ST depression; this indicates a worse prognosis
Transient ST elevation
T-wave changes.
Be aware that the ECG may be normal in more than 30% of patients.[1]
Record additional leads if the standard leads are inconclusive, if total vessel occlusion is suspected, or in cases of suspected inferior STEMI.[7]
Leads V 7-V 9 may detect left circumflex artery occlusion and leads V 3R and V 4R may detect right ventricular myocardial infarction.[7]
Order repeated resting ECGs if the patient has recurrent symptoms or you are unsure about the diagnosis.[7][63]
Always compare the current ECG with previous ECGs where possible.[63]
How to record an ECG. Demonstrates placement of chest and limb electrodes.
[Figure caption and citation for the preceding image starts]: Position of ECG leads V7-V9Image used with permission from BMJ 2002;324:831 [Citation ends].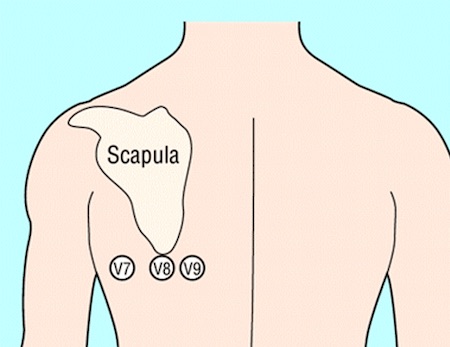 [Figure caption and citation for the preceding image starts]: Position of right precordial ECG leads V3R and V4RImage used with permission from BMJ 2002;324:831 [Citation ends].
[Figure caption and citation for the preceding image starts]: Position of right precordial ECG leads V3R and V4RImage used with permission from BMJ 2002;324:831 [Citation ends].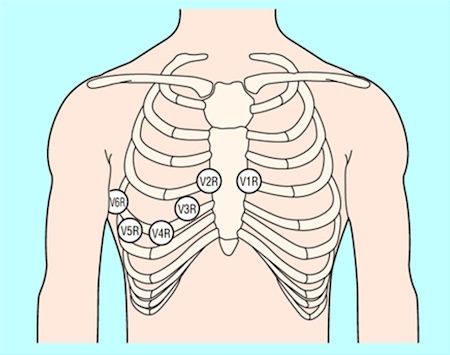 [Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].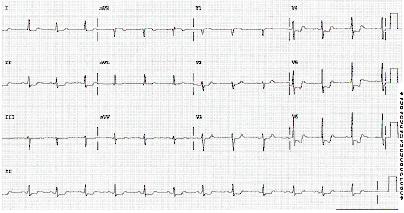 [Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing inferolateral ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing T wave inversion in leads V1-V4, III and aVF.BMJ Learning/Professor Kevin Tanner; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing T wave inversion in leads V1-V4, III and aVF.BMJ Learning/Professor Kevin Tanner; used with permission [Citation ends].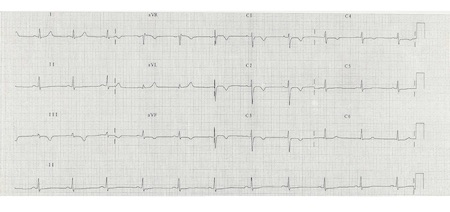
Result
ST depression (indicates a worse prognosis)
transient ST elevation
T-wave changes
high-sensitivity troponin
Test
Measure high-sensitivity cardiac troponin (hs-cTn) immediately after presentation and obtain results within 60 minutes in all patients with suspected acute coronary syndrome (ACS).[7]
Use a diagnostic algorithm: the European Society of Cardiology recommends using the 0/1 hour or 0/2 hour 'rule in' and 'rule out' algorithms, which classify patients into one of three pathways according to the results of their hs-cTn values at 0 hours (time of initial blood test) and 1 hour or 2 hours later.[7]
Rule-out pathway: for very low initial hs-cTn or no increase after 1/2 hours: these patients may be appropriate for early discharge and outpatient management.
Rule-in pathway: for high initial hs-cTN or an increase after 1-2 hours: most of these patients will require hospital admission and invasive coronary angiography.
Observe pathway: if neither of the above criteria is met: check hs-cTN at 3 hours and consider echocardiography.
In practice, patients with a raised hs-cTN presenting in the accident and emergency department are often referred to cardiology before a second troponin test.
Cut-off values for hs-cTn are dependent on the assay used; check your local protocol.[7]
Use the algorithm in the context of other clinical criteria such as a detailed history of the chest pain and any ECG findings.[7]
Some patients may need an additional measurement of troponin at 3 hours (e.g., if the first two hs-cTn measurements of the 0/1 algorithm are inconclusive, and no alternative diagnoses explaining the condition have been made).
The higher the hs-cTn at presentation, the higher the risk of death.[7]
Practical tip
Reassess the patient if they have a raised hs-cTn.
Troponin can be acutely raised due to other causes such as myocarditis, aortic dissection, or acute pulmonary embolism.[63]
Chronic elevation of high-sensitivity troponin is also common in patients with renal dysfunction and heart failure.[1][7]
Troponin levels may remain elevated for 1-2 weeks following recent myocardial infarction and/or percutaneous coronary intervention.
Interpret hs-cTn in the context of the clinical scenario.
Result
dynamic elevation above the 99th percentile[7]
chest x-ray
Test
The National Institute for Health and Care Excellence (NICE) recommends ordering a chest x-ray only if you suspect other diagnoses or to rule out complications of ACS.[63] However, in our expert’s opinion you should order a chest x-ray for all patients with acute chest pain to look for other causes, such as pneumothorax or a widened mediastinum in aortic dissection, or complications of ACS such as pulmonary oedema due to heart failure.
Practical tip
Ensure an ECG is recorded and interpreted before considering a chest x-ray. If the ECG indicates ST-elevation myocardial infarction, refer the patient immediately to cardiology for consideration of primary percutaneous coronary intervention to avoid the delay that may be associated with requesting a chest x-ray.
Result
other causes of acute chest pain, such as pneumothorax or a widened mediastinum in aortic dissection
complications of ACS, such as pulmonary oedema due to heart failure
full blood count
Test
Check full blood count to evaluate:
Thrombocytopenia to estimate risk of bleeding; NSTEMI treatment increases the risk of bleeding
Possible secondary causes of NSTEMI (i.e., secondary blood loss, anaemia).
Result
normal, anaemia, thrombocytopenia
urea, electrolytes, and creatinine
Test
Measure renal function to:
Determine serum creatinine and estimated glomerular filtration rate (eGFR); these are key elements in assessing the Global Registry of Acute Coronary Events (GRACE) risk score.[7] [ GRACE Score for Acute Coronary Syndrome Prognosis Opens in new window ] See Risk assessment in Management recommendations.
Prevent contrast-induced nephropathy if an invasive strategy is planned in a patient with chronic kidney disease (CKD).[1][7]
Be aware that a patient with CKD may have a chronically raised troponin.[1] Patients with CKD may also have electrolyte abnormalities that can cause ECG abnormalities.[7]
Result
baseline levels
liver function tests
Test
Measure liver function to include in the assessment of bleeding risk before starting anticoagulation.[7]
Result
baseline levels
blood glucose
Test
Check blood glucose in any patient with known diabetes or hyperglycaemia on admission to hospital, regardless of a history of diabetes.[7][61]
Monitor blood glucose levels frequently if the patient has known diabetes or hyperglycaemia on admission.[7][61]
Manage hyperglycaemia in patients admitted with confirmed NSTEMI by keeping blood glucose <11 mmol/L (198 mg/dL) while avoiding hypoglycaemia.[61] See Management of hyperglycaemia in Management recommendations.
Result
normal, hyperglycaemia
C-reactive protein
Test
NICE does not recommend using C-reactive protein (CRP) to diagnose an ACS.[63] However, in our expert’s opinion, CRP is commonly ordered to rule out other causes of acute chest pain (e.g., pneumonia).
Result
elevated if infection present
Investigations to consider
echocardiography
Test
Organise urgent echocardiography for any patient with signs of acute heart failure or haemodynamic instability or who is in cardiac arrest.[7] This should only be performed by those with specialist training.
Result
regional wall motion abnormalities
left ventricular systolic function
alternative causes of chest pain such as acute aortic disease or right ventricular dysfunction suggestive of acute pulmonary embolism[7]
invasive coronary angiography (ICA)
Test
Get urgent input from a senior colleague or cardiology if the patient is clinically unstable or has any very high-risk features (as outlined below) to arrange immediate invasive coronary angiography (with the intent to perform revascularisation by percutaneous coronary intervention [PCI] if indicated).[61] Do not wait for the results of troponin testing.[7] This includes any patient with:[7][61][62]
Ongoing or recurrent pain despite treatment
Haemodynamic instability (low blood pressure or shock) or cardiogenic shock; see Shock
Recurrent dynamic ECG changes suggestive of ischaemia
Acute left ventricular failure, presumed secondary to ongoing myocardial ischaemia; see Acute heart failure
A life-threatening arrhythmia (ventricular tachycardia or ventricular fibrillation) or cardiac arrest after presentation; see Sustained ventricular tachycardias
Mechanical complications such as new-onset mitral regurgitation.
An inpatient invasive strategy is recommended for most patients presenting with non-ST-elevation acute coronary syndrome (NSTE-ACS); the timing of this is guided by an early risk assessment, which divides patients into very high risk, high risk, or non-high risk.[7] High-risk patients should have ICA within 24 hours.[7] Patients without high-risk features can be managed based on clinical suspicion; conservative management without early angiography may be an option for very low-risk patients.[7][61]
Perform further risk assessment after a final diagnosis has been made and treatment administered. For more information, see Risk assessment in Management recommendations.[7]
Result
acute occlusion or critical stenosis
Use of this content is subject to our disclaimer
