Authors: Ricardo Catumbela, Ryan Linn, Aminah Amer, Faraz Sethi, Russel stocker, Dr Irfan Ahmed
Exercise-induced leg pain
Exercise-induced leg pain (ELP) is a widespread condition among exercising adults that can hinder their ability to participate in physical activities or affect their performance. In primary care, understanding the common causes of ELP may help achieve an accurate diagnosis early and mitigate its physical, economic, and social impact burden.
Exercise-induced leg pain (ELP) has a broad aetiology, with potential causes including vascular, musculoskeletal, neurological, and pharmacological factors. A sports medicine-focused history and examination can help narrow the differential diagnoses and guide further management and specialist workup in the clinic.
What is chronic exertion compartment syndrome?
hronic exertional compartment syndrome (CECS) is an underdiagnosed condition that leads to reversible pain and neuromuscular symptoms in specific muscle compartments during or shortly after exercise. Approximately 20% of patients suffering from exercise-related chronic anterior lower leg pain are diagnosed with CECS, with 70% of these being runners. Young males aged 20 to 25 are more frequently affected than their female counterparts. (1–3)
Table 1: High risk sports populations affected by CECS (1-3)
| Commonly affected groups/High-risk population/High-risk groups | |
| Upper Limb | Rowers, Tennis players, Motorcyclists, etc. |
| Lower Limb | runners, dancers, gymnasts and military personnel |
In healthy individuals, exercise temporarily raises intramuscular pressure, which returns to normal levels once the activity stops. However, it is believed that in affected individuals, exercise-induced muscle growth and increased vascular demand cause abnormal compartment pressure, reducing both arterial and venous blood flow and compressing peripheral nerves, leading to ischemic pain and neurological symptoms. (2, 4, 5) Our knowledge of the pathophysiology of CECS and the influence of factors such as diminished fascial compliance, myopathies, and microtrauma is still limited.
Table 2: Common presentation of patients suffering from CECS (4)
| Common signs/symptoms / Common complaints | |
| Pain “cramping”, “aching”, “burning” | Paraesthesia “pins and needles” |
| Swelling “feeling tight” | Muscle Weakness “foot-drop” |
What featured of the history are particularly important in diagnosis?
Over 90% of CECS cases impact the lower limb, particularly the anterior compartment. Patients with CECS typically experience localised, exercise-induced pain, often described as tightness, cramping, or aching, which may be accompanied by paraesthesia, hyperesthesia, and weakness. (5)
Symptoms occur at a particular exercise intensity or duration, with patients often describing the urge to “stop and stretch”. Symptoms are usually relieved by rest, though recurrence occurs with the resumption of the inducing exercise. (5)
Figure 1: Key features of CECS

The existence of red flag symptoms requires prompt assessment and referral to urgent medical services for specialised investigations.
Table 3: Red flag symptoms to be screened for in primary care or by FCP/APP (6)
| Red Flag Symptoms: |
| Pain not relieved by rest |
| Persistent neurovascular compromise |
| New urinary and/or faecal incontinence |
| Concomitant lower back pain |
| Pain at night |
| Unintentional weight loss |
| Excessive sweating |
| Fever and/or systemic symptoms |
| History of previous malignancy |
What other conditions should I consider during the assessment?
Patients with a history of metabolic syndrome face a higher risk of developing vascular or neuropathic syndromes due to atherosclerosis and neuronal degeneration.(7) Purely neurogenic disorders may arise from autoimmune conditions, alcohol abuse, hypothyroidism, liver or kidney disease, viral infections, or heavy metal poisoning such as mercury or lead. (8) Primary care clinicians should consider laboratory blood tests guided by a focused history and known risk factors (Table 3).
Table 4: Blood tests should be considered in primary care before referral to secondary care
| Blood test | When to be concerned |
| FBC | Abnormalities in the blood count including anaemia or sinister causes |
| U&Es | Electrolyte imbalances and/or kidney disease |
| LFTs | Deranged liver function including ALP |
| TFTs | Deranged thyroid function |
| HbA1C | Poorly controlled diabetes |
| CK | Raised creatinine kinase (statins/myopathy) |
| Lipids | Raised cholesterol (PVD) |
| Vitamin D | Low vitamin D – common in the UK |
| Bone profile including Ca, Phosphate + ALP | Low Ca and/or phosphate can imply longstanding severe vitamin D deficiency
Can help indicate if the patient may have Osteomalacia |
| Parathyroid hormone | Raised levels may indicate increased bone activity |
| Ferritin, B12 and folate | The patient may be deficient in other vitamins and minerals |
| Anti-TTG (coeliac serology) | Cause for malabsorption |
Vitamin D deficiency (see Supplementary Table 1) and hypophosphatemia, hypocalcaemia, or osteopenia are treatable medical risk factors that require screening. In athletes at risk for RED-S (Relative Energy Deficiency in Sport), bone stress injuries (BSI) should be considered and managed through a comprehensive approach that includes exercise, metabolic health, and strategies to enhance bone health. (9) Furthermore, Chronic Exertional Compartment Syndrome (CECS) may exhibit symptoms that resemble the initial phases of the Bone Stress Injury (BSI) spectrum, including periostitis and Medial Tibial Stress Syndrome (MTSS).
Table 5 – Differentials of exercise-induced leg pain. (10,11)
| Aetiology | Common differentials | Clinical Signs on Examination | Risk Factors |
| Vascular | Peripheral Vascular Disease (Atherosclerosis) Peripheral artery dissection Popliteal Artery AneurysmFunctional Popliteal Artery Entrapment Syndrome Deep Venous Thrombosis |
Absent peripheral pulses Ankle Brachial Pulse Index (ABPI) after exercise: <0.5 – severe arterial disease 0.5-0.8 – arterial disease or mixed arterial and venous diseasePain on the posterior compartment during passive dorsiflexion of the foot with the knee extended |
Smoking history, Obesity, Diabetes, Hyperlipidaemia, Hypertension, Ischemic Heart Disease, Cerebral Vascular Accidents, IV Drug Use History |
| Muscular | Fascial Herniation
Myopathy Tendinopathy |
Bruising or haematomas
Blisters Lumps or visual deformities |
History of recent trauma, sprain, crush injury (excessive force or pressure)
Recent viral infection |
| Bone | Bone stress injury
Bone stress fracture Periostitis (Medial Tibial Stress Syndrome) Osteomyelitis Tumour |
Pain on bone palpation. Pain on the “bone squeeze test” | Low Serum Vit D, Hypocalcaemia
Hypophosphatemia, Eating disorders, Malabsorption, Female Gender, Performing artist |
| Spine | Vertebral Fractures Spinal Cord Compression Cauda Equina Syndrome RadiculopathyDisc prolapse Discitis Tumour |
Lower motor neuron signs
Upper motor neuron signs Pain worsening on straight leg raise with “big toe” dorsiflexion or during the slump test Spinal tenderness or deformity |
Older age (>50 years old), History of back pain or disc disease, Previous spinal interventions, Previous spinal trauma, Bacteraemia or presence of implanted devices (i.e. heart valve, pacemakers, etc.) |
| Superficial/Peripheral nerve impingement | Neuropathy of Lateral Cutaneous nerve, Superficial Peroneal Nerve, Common Peroneal Nerve or Sural Nerve (Diabetic amyotrophy, Entrapment) | Lower motor neuron signs with relevant myotomal/dermatomal distribution.
Tinel’s sign positive: Hyperglycaemia and/or Raised HbA1C |
Diabetes, Hypothyroidism, Hepatic or Renal failure, ETOH overuse,
Autoimmune diseases (Sjogren, Lupus, RA, GBS, CIDP, Vasculitis), Infections (Shingles, EBV, Hep B and C, Leprosy, Lyme disease, diphtheria, botulism, HIV), Low serum B1, B3, B6, B12, E vitamins, Lead and Mercury intoxication |
| Other neurogenic causes | Myasthenia Gravis | Slurred speech, dysphagia, generalised weakness (including facial nerves), shortness of breath | Autoimmune diseases, History of a Thymoma |
| Medication-related | Statins, Beta blockers, Beta-2 agonists, Diuretics (esp. thiazides, loop diuretics), ACEi, ARBs, Antipsychotics | Medication history |
Figure 2 – Differentials of exercise-induced leg pain. (10,11)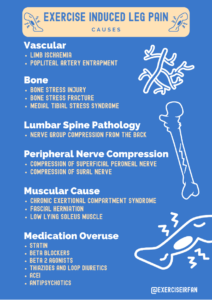
Primary care focussed assessment for chronic exertion compartment syndrome
The physical examination of patients with CECS is often unremarkable when undertaken at rest, as symptoms typically emerge only during particular physical activities. Given that the increase in intra-compartmental pressure is specific to exercise, the assessment should be carried out during or after the patient’s symptom-inducing exercise.
Figure 3 – Focussed physical exam, helpful in assessing ELP in primary care
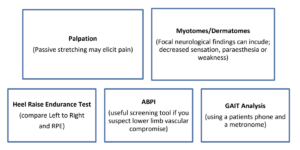
When evaluating CECS patients, initial contact practitioners, such as physiotherapists or primary care physicians, should conduct a thorough physical examination and collect medical history before arranging targeted investigations. If a vascular issue is suspected, the Ankle Brachial Pulse Index is a straightforward primary care test that can be performed before and after exercise to assess for vascular compromise. Additionally, practitioners should also check for widespread pain syndromes that may mimic musculoskeletal pain.
Table 6 – Clinical examination findings in CECS
| Clinical Examination | Signs |
| Inspection | Pallor
Swelling Myofascial Herniations/Fasciculations/Deformity |
| Palpation | Firmness & tenderness along the myofascial compartment
Faint or absent distal pulses in severe cases (i.e. Popliteal, Posterior Tibial Artery, Dorsalis Pedis Artery) Poikilothermic |
| Neurological | Localised reduced sensation (i.e. dorsum of the foot, 1st web space)
Localised muscle weakness (i.e. foot drop) |
Which patients should I refer on?
When managing patients with CECS, it is essential to consider their goals and needs. A conservative therapy trial lasting 6 to 12 weeks is generally recommended, with an effectiveness evaluation after 3 to 6 months. If conservative methods do not succeed, or if the patient experiences ongoing debilitating symptoms that hinder physical activity, they should be referred to a specialist in sports medicine or orthopaedics.
Intra-compartmental pressure monitoring (ICP), post-exertion magnetic resonance imaging, and near-infrared spectroscopy are valuable tools for diagnosing chronic exertional compartment syndrome (CECS). Although a definitive consensus has not been reached, ICP continues to be the most widely used in clinical settings. Various exercise and procedural protocols exist for measuring ICP and collectively indicate that CECS patients experience higher resting pressures before and after exercise than control subjects. (4, 10)
Figure 4 – Infographic on the work up of ELP patients in primary care

What treatment options are available?
-
Conservative Management
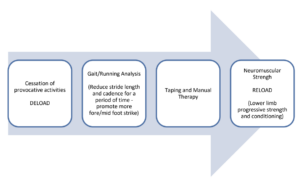
Non-operative management typically begins with the cessation of the provoking exercise, although patients may resist this, as it could jeopardise their careers. Altered gait biomechanics and running style significantly contribute to the pathophysiology of CECS. (11)
Gait re-training should ideally involve objectively assessing running and employing clinical cues to guide changes to alleviate symptoms.
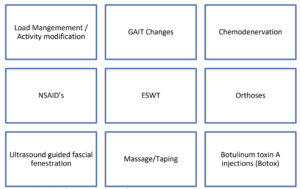
Figure 5 – Conservative options for the management of CECS
Clinicians should concentrate on one aspect of gait re-training at a time, evaluate its effect on symptoms, and attempt an alternative strategy or combine techniques if no improvement is observed. Beginning with adjustments to cadence is frequently effective. (11)
Using a treadmill with video analysis may be helpful. It ensures consistent speed and incline throughout, reducing external variables. Cadence adjustments can be cued with online metronomes or mobile apps.
Table 7 – Examples of gait retraining strategies
| Strategy | Assessment/Measurement | Aim | Clinical Cues/Performance |
| Cadence | Count steps taken during a timed 60 second test
Treadmill helps to maintain consistent speed |
165-180 steps per minute | Set metronome
Maintain a consistent running speed Run to metronome beat without changing speed |
| Alter ground reaction forces | Listen to foot strike on treadmill, is it loud, is it equal? | Reduce forces on foot strike | Cues:
Shorten step length Avoid over-striding (reaching the foot far out in front) Aim to land on the mid-foot Aim to land as softly as possible |
| Foot landing position | Video analysis – pause frame on foot strike
Observe trainers for wear patterns |
Mid to forefoot strike | Cue:
Imagine lifting the heels 2-3cm higher than usual at heel off. Aim to land with weight on the middle of the foot. |
Figure 6 – A stepwise approach to rehabilitating a CECS patient using conservative measures from deloading and gait retraining to strength and conditioning
Alternative non-surgical treatment options include non-steroidal anti-inflammatory drugs, chemo-denervation, extracorporeal shockwave therapy, orthotics, ultrasound-guided fascial fenestration, botulinum toxin A injections, and taping.
2. Surgical Management
It is advisable to explore all non-surgical options prior to considering operative management, based on the patient’s goals. The standard surgical intervention involves performing a fasciotomy on one or more compartments. This procedure can be carried out through open surgery, endoscopically, via a single small incision, percutaneously, or even with ultrasound guidance.
Figure 7 – Evolution of fasciotomy techniques: From traditional open methods to minimally invasive, ultrasound-guided procedures

Recovery rates, the ability to return to the same activity level, and symptom resolution vary across studies. Recurrence rates can reach 45% (12), with nearly 20% of patients requiring further surgeries. Therefore, it is essential to categorise risk factors for CECS, as mixed cases involving mechanical or metabolic factors are less likely to achieve complete recovery following surgical intervention. Surgical complications, which include scarring, nerve damage, infection, haemorrhage, vascular injury, and thromboembolism, occur in about 16% of cases (12).
References
- George CA, Hutchinson MR. Chronic Exertional Compartment Syndrome. Clin Sports Med. 2012 Apr;31(2):307–19.
- Bonasia DE, Rosso F, Cottino U, Rossi R. Exercise-induced leg pain. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015 Jul;2(3):73–84.
- Schubert AG. Exertional compartment syndrome: review of the literature and proposed rehabilitation guidelines following surgical release. Int J Sports Phys Ther. 2011 Jun;6(2):126–41.
- Tzortziou V, Maffulli N, Padhiar N. Diagnosis and Management of Chronic Exertional Compartment Syndrome (CECS) in the United Kingdom. Clinical Journal of Sport Medicine. 2006 May;16(3):209–13.
- Velasco TO, Leggit JC. Chronic Exertional Compartment Syndrome: A Clinical Update. Curr Sports Med Rep. 2020 Sep;19(9):347–52.
- C. Ramanayake RPJ, K. Basnayake BMT. Evaluation of red flags minimizes missing serious diseases in primary care. J Family Med Prim Care. 2018;7(2):315.
- Di Pietro P, Izzo C, Carrizzo A. Editorial: The role of metabolic syndrome and disorders in cardiovascular disease. Front Endocrinol (Lausanne). 2023 Oct 31;14.
- Chen P, Miah MR, Aschner M. Metals and Neurodegeneration. F1000Res. 2016 Mar 17;5:366.
- Jasty NM, Dyrek P, Kaur J, Ackerman KE, Kraus E, Heyworth BE. Evidence-Based Treatment and Outcomes of Tibial Bone Stress Injuries. Journal of the Pediatric Orthopaedic Society of North America. 2021 Nov;3(4):372.
- Bosnina F, Padhiar N, Miller S, Girotra K, Massoura C, Morrissey D. Developing a diagnostic framework for patients presenting with Exercise Induced Leg Pain (EILP): a scoping review. J Foot Ankle Res. 2023 Jan 21;16(1).
- Padhiar N, Malliaropoulos N, Lohrer H. Exercise-induced leg pain in sport. Br J Sports Med. 2015 Dec 1;49(24):1546–7.
Supplementary materials
Figure 8 – Vitamin D Treatment guidelines
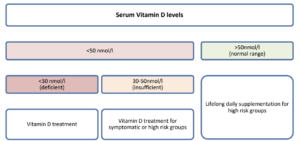
The two primary sources of vitamin D are sunlight exposure and specific food groups. However, certain populations are at higher risk for vitamin D deficiency and require particular attention (table 8)
Table 8 – High-risk groups for vitamin D deficiency.
| At risk populations: |
| Infants 0-3 years old |
| Pregnant and breast-feeding women |
| Adults aged over 65 years old |
| Housebound individuals |
| Individuals who cover their skin for cultural or religious reasons |
| South-Asian, African and African-Caribbean individuals, specially women and children |
Patients in at-risk groups must be educated on the importance of lifelong vitamin D supplementation to ensure compliance. Clinicians should provide culturally sensitive advice, especially when discussing how darker skin and covering up relate to vitamin D deficiency. Some patients may avoid certain brands of cholecalciferol due to gelatine content, so alternatives should be offered. Mothers, pregnant, and breastfeeding women should be informed about Healthy Start supplements and how to access them at a reduced or waived cost.
Table 9 – Vitamin D replacement dosage according to age as per NICE CKS recommendations. Find more information on: https://cks.nice.org.uk/topics/vitamin-d-deficiency-in-adults/management/management/
| Vitamin D Treatment – Loading and Maintenance Dosage according to age | ||
| Age | Loading | Maintenance |
| 1-6 months | 3000 IU cholecalciferol daily for 12 weeks | 400-600 units daily all ages |
| 6 months -12 years | 6000 IU cholecalciferol daily for 12 weeks | |
| 12-18 years | 10000 IU cholecalciferol daily for 12 weeks | |
| Over 18 years | 40000 IU per week for 7 weeks | 800-2000 units daily after loading dose.
Consider up to 4000 units per day for high-risk groups |
| *rule out chronic liver disease, chronic kidney disease and hypercalcaemia
** if using high dose loading treatment – re-check calcium 1 month after initiating treatment |
||
Author information
Dr Ricardo Catumbela
Medical Doctor
Research Director – Optima Performance LinkedIn: Dr Ricardo Catumbela
Dr Ryan Linn
Resident Doctor
University Hospitals North Midlands X: @ryan_linn_
Dr Aminah Amer
General Practice Consultant Manchester Metropolitan University LinkedIn: Dr Aminah Amer
Faraz Sethi
Specialist MSK Physiotherapist
APP Advanced Practitioner Physiotherapist (NHS) www.thefarazzledphysio.co.uk
Russell Stocker
Physiotherapist
Stocker’s Physiotherapy https://www.facebook.com/share/38iT5sbasJ8ieZVx/?mibextid=LQQJ4d www.stockersphysiotherapy.co.uk
Dr Irfan Ahmed
Consultant in Musculoskeletal, Sport & Exercise Medicine
X: @ExerciseIrfan www.mskplaybook.com