Diagnosis and management of hypertension in pregnancy: summary of updated NICE guidance
BMJ 2019; 366 doi: https://doi.org/10.1136/bmj.l5119 (Published 09 September 2019) Cite this as: BMJ 2019;366:l5119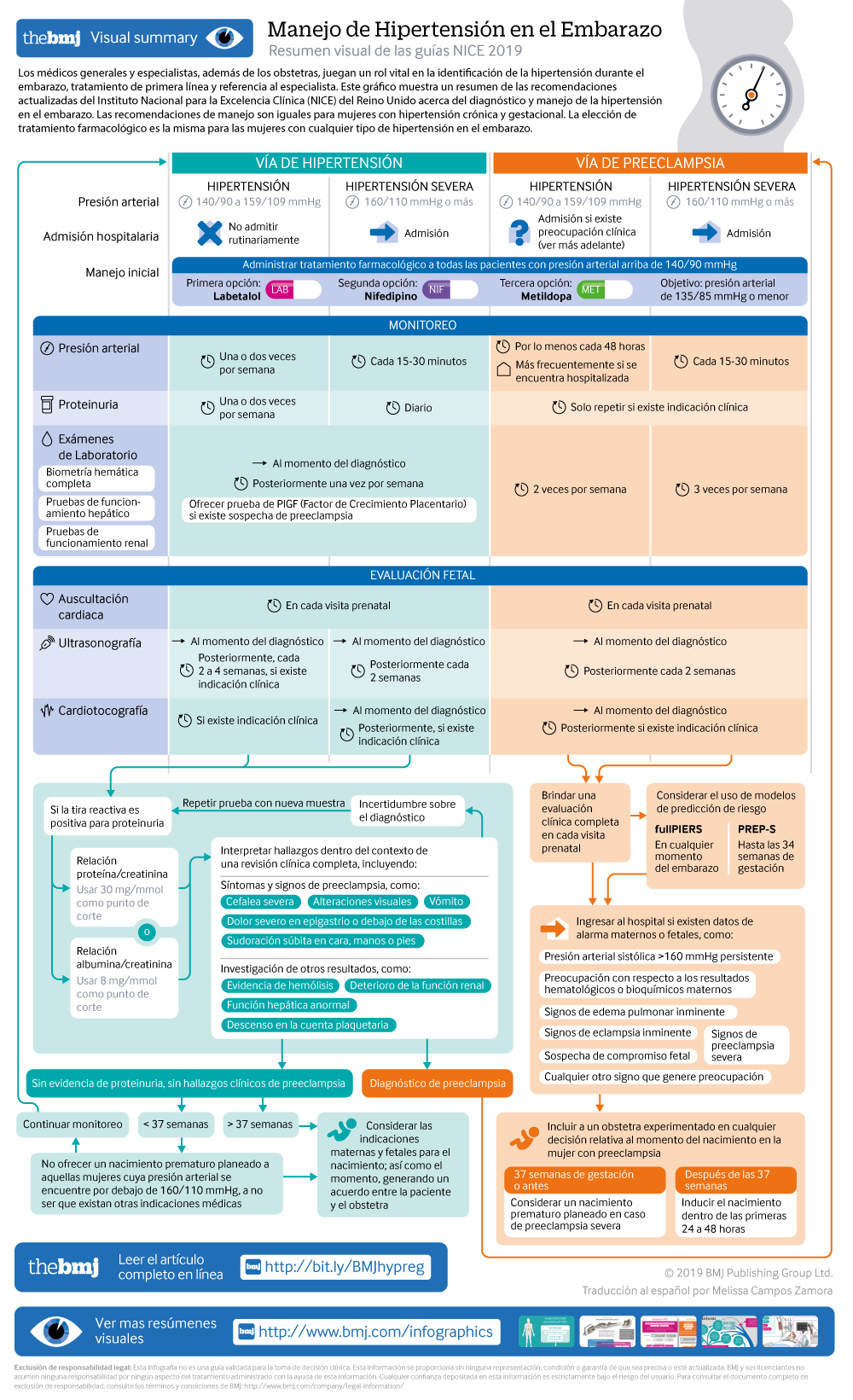
Visual summary: Resumen visual
Spanish version: Versión en español
- Katie Webster, senior systematic reviewer1,
- Sarah Fishburn, chair of guideline committee1,
- Mike Maresh, clinical adviser1,
- Sarah C Findlay, lay member,
- Lucy C Chappell, topic advisor and NIHR research professor in obstetrics2
- on behalf of the Guideline Committee
- 1National Guideline Alliance, Royal College of Obstetricians and Gynaecologists, London
- 2King’s College London
- Correspondence to: L C Chappell lucy.chappell@kcl.ac.uk
What you need to know
Hypertension affects about 10% of pregnant women, including those with pre-existing hypertension, chronic hypertension that is first diagnosed during pregnancy, and hypertension related to pregnancy (gestational hypertension and pre-eclampsia)
Target blood pressure during the antenatal period should be 135/85 mm Hg for women with hypertension during pregnancy
Hypertension during pregnancy is associated with an increased risk of hypertension and cardiovascular disorders in later life. Women should be offered appropriate lifestyle and dietary advice to minimise this risk
Hypertension in pregnancy is a common condition, affecting about 10% of pregnant women. This includes women with chronic hypertension—which may be diagnosed before pregnancy or in the early stages of pregnancy (<20 weeks’ gestation)—and women with hypertension related to pregnancy (gestational hypertension and pre-eclampsia) (see box 1). If not identified and treated, hypertension can lead to adverse events for both the woman and her baby, including increased risk of maternal stroke, lower birth weight, and increased risk of the baby requiring neonatal intensive care.
Definitions for hypertensive disorders of pregnancy
Chronic hypertension—Hypertension that is present at the booking visit or before 20 weeks’ gestation, or if the woman is already taking antihypertensive medication when starting maternity care. It can be primary or secondary in aetiology
Gestational hypertension—New hypertension presenting after 20 weeks of pregnancy without significant proteinuria
Pre-eclampsia—New onset hypertension (>140 mm Hg systolic or >90 mm Hg diastolic) after 20 weeks of pregnancy and the coexistence of one or both of the following new-onset conditions:
Proteinuria (urine protein:creatinine ratio ≥30 mg/mmol, or albumin:creatinine ratio ≥8 mg/mmol, or ≥1 g/L [2+] on dipstick testing)
Other maternal organ dysfunction, including features such as renal or liver involvement, neurological or haematological complications, or uteroplacental dysfunction (such as fetal growth restriction, abnormal umbilical artery Doppler waveform analysis, or stillbirth)
General practitioners and specialists other than obstetricians play a vital role in the identification of hypertension during pregnancy, first …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £184 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£50 / $60/ €56 (excludes VAT)
You can download a PDF version for your personal record.
