Abstract
An increased understanding of the interrelations between depressive symptoms among older populations could help improve interventions. However, studies often use sum scores to understand depression in older populations, neglecting important symptom dynamics that can be elucidated in evolving depressive symptom networks. We computed Cross-Lagged Panel Network Models (CLPN) of depression symptoms in 11,391 adults from the English Longitudinal Study of Ageing. Adults aged 50 and above (mean age 65) were followed over 16 years throughout this nine-wave representative population study. Using the eight-item Center for Epidemiological Studies Depression Scale, we computed eight CLPNs covering each consecutive wave. Across waves, networks were consistent with respect to the strength of lagged associations (edge weights) and the degree of interrelationships among symptoms (centrality indices). Everything was an effort and could not get going displayed the strongest reciprocal cross-lagged associations across waves. These two symptoms and loneliness were core symptoms as reflected in strong incoming and outgoing connections. Feeling depressed was strongly predicted by other symptoms only (incoming but not strong outgoing connections were observed) and thus was not related to new symptom onset. Restless sleep had outgoing connections only and thus was a precursor to other depression symptoms. Being happy and enjoying life were the least central symptoms. This research underscores the relevance of somatic symptoms in evolving depression networks among older populations. Findings suggest the central symptoms from the present study (everything was an effort, could not get going, loneliness) may be potential key intervention targets to mitigate depression in older adults.
Similar content being viewed by others
Introduction
Depression contributes significantly to the global disease burden [1] and is common among people aged 50 years and above in Europe and North America, with meta-analytic lifetime prevalence estimates of 16.5% [2]. More recent meta-analyses of individuals aged 60 years and above indicate that the global prevalence of depression is 28.4% according to questionnaire cut-offs [3] and 13.3% for a diagnosis of major depression [4]. However, depression prevalence is heterogenous across studies, countries, and age groups [2, 3, 5, 6]. In older populations, depression often remains unrecognized, with undertreatment leading to sustained impairment [7]. Under-recognition may be attributable to a substantial variability in the presentation and manifestation of depressive symptoms across the lifespan [8]. In older adults, depression often presents with more somatic symptoms than in younger populations [6, 9], yet current diagnostic systems conceptualize depression as a unitary, unchanging construct over the lifespan [10, 11]. To date, depression in older populations has been predominated by studies of cumulative sum scores [12], which can hide false assumptions that symptoms equally contribute to an underlying depression construct [13]. However, individual depressive symptoms have displayed differential associations with risk factors [14], comorbidity [15], and levels of impairment [16].
To elucidate the inter-relationship of depression symptoms, the network approach has been applied across different ages and populations [17, 18]. Instead of construing depression as a common factor with interchangeable indicators of disorder, the network approach defines mental disorders as a casual system of mutually interacting symptoms [19]. Analysis is focused on these symptoms; their importance (i.e., centrality) and interrelations can be examined empirically [20]. Core symptoms can be tested for clinical relevance in intervention studies [21, 22].
To date, network analyses have provided insight into the relative importance of different depressive symptoms across various populations [23], but network studies of depression in older populations are scarce. The few available studies in adults ages 50 and above point to the centrality of the symptom depressed mood [24,25,26,27,28]. However, these studies were cross-sectional or, despite being longitudinal, did not identify the directionality of symptoms. To test whether symptom relationships are temporal, network analyses must be conducted across a series of longitudinal models. This discerns whether some symptoms precede other symptoms, a central claim of network analysis. For instance, sleep problems may lead to concentration problems, which, in turn, could intensify feelings of anhedonia [19]. Identifying precursor symptoms has important implications as these symptoms can be targeted to stop future symptom activation. Temporal patterns among depressive symptoms were discerned in one longitudinal study of adults ages 50 and above where feeling sad and depressed mood were central symptoms which were predicted by many other prior symptoms [28]. However, this study aggregated data across waves and thus it remains unclear whether specific symptoms have a different impact at different stages during the ageing process [28].
Given the above limitations, a comprehensive examination of depressive symptom networks over time in older populations is warranted. This can advance knowledge of depression in older adults in two ways. First, it may reveal the existence of consistent network structures across different time periods, which could help to identify robust and replicable effects. This would provide crucial insight as network results are not always perfectly replicable both cross-sectionally and over time [17, 29, 30]. Second, this work may highlight unique network patterns that emerge across specific time points, particularly in instances where significant developmental events occur, such as retirement, shifts in social roles, or widowhood [6]. If consistent symptom patterns emerge over time, this may inform broad prevention programs, but if specific symptom constellations are limited to certain ages [8], this may inform more tailored approaches [6].
Specifically, it is important to discern the role of the hallmark symptom depressed mood across time, as this is one of two key symptoms required for depression diagnoses [10, 11]. However, longitudinal network analysis findings suggest that at the point of experiencing depressed mood many other symptoms are likely to have already been activated [28, 31], and thus will have already been causing functional impairment. Accordingly, the precursor symptoms to depressed mood may have relevance as warning signs of potential activation of diagnosable depression [32].
The role of loneliness in older adult depression networks is also understudied. While not a core symptom in standardized depression diagnoses [10, 11], older adults are often socially isolated and may be affected by separation, bereavement, and widowhood [6]. Increased loneliness in older adults has been associated with greater depressive symptom development, and conversely more depressive symptoms can reinforce social withdrawal and isolation [33]. Given the significance of loneliness among older adults [34], this symptom needs investigation within evolving depression networks.
Likewise, depression networks in older adulthood have not included somatic symptoms relating to fatigue (could not get going anymore; everything was an effort). Compared with younger cohorts, older adults are more likely to have reduced physical functioning due to chronic diseases or multiple comorbid health-related conditions [6], and from this may experience feelings of fatigue or increased burden. Likewise, disturbed sleep needs further study in older adults, as sleep is of high therapeutic relevance and influences depression treatment outcomes [35, 36]. In a longitudinal study, trouble sleeping had some outgoing connections but almost no incoming associations, indicating that this symptom may be implicated in the initiation of symptom cascades [28]. This could reflect a somatic pathway toward depression [8] with many outgoing unidirectional connections of somatic symptoms to subsequent mood-related symptoms [31]. Thus, understanding the role of these symptoms in longitudinal depression networks in older adults is key.
Present study
The literature currently lacks a developmental perspective of how depressive symptoms operate in evolving longitudinal depression networks in older adults. Thus, we sought to investigate temporal depressive symptom constellations using data from the English Longitudinal Study of Ageing (ELSA), a nine-wave representative study of the English population above 50 years of age, with mean ages ranging from 65 to 76. Given the high and heterogenous levels of depression prevalence across age and particularly after age 50 [3, 5], this allows us to gauge whether the development of depressive symptoms is driven by different symptom dynamics across time in older adults. The present contribution focuses on the eight-item Centre for Epidemiologic Studies Depression Scale (CES-D-8), a psychometrically sound measure to assess depressed affect (enjoyed life, felt depressed, happy, lonely, and felt sad) and somatic complaints (everything was an effort, sleep was restless, and I could not get going) [37]. Using eight consecutive Cross-Lagged Panel Network Models (CLPN; 35), we aimed to disentangle how each of the CES-D-8 depressive symptoms may be predictive of, or predicted by, other depressive symptoms, and thus how central they are to depression in older adults. Based on the existing literature, we expected feeling depressed to emerge as one of the most central symptoms [28, 38]. Given the scarceness of longitudinal studies in older populations, we did not specify further a priori hypotheses.
Methods
Participants
The ELSA study focused on individuals aged 50 and above residing in private households in England [39]. The sample was drawn from participants of the Health Survey for England (HSE), which was boosted to ensure the representation of ethnic minorities. For ELSA, HSE households were excluded from the sampling frame if there was no adult aged 50 or older who had agreed to be contacted in the future. The remaining households provided the foundation for the ELSA Wave 1 sample that enrolled participants in 2002/2003. The study is representative of the population aged 50 years and older and consists of nine waves that took place once every two years. A multistage stratified probability sampling was used, and samples were refreshed over time to maintain representativeness. Core sample members are the 11,391 adults born on or before 29 February 1952 who initially took part in HSE. To allow for comparability of the networks, we focus on the core sample members with repeated-measures data in the present analyses. Demographic characteristics, assessment year, and participation rate for each ELSA wave are depicted in Table 1. Ethical approval was granted by the National Research Ethics Service (MREC/01/2/91). Participants provided informed consent. Data are openly available via the UK Data service. Our secondary data analysis was not preregistered (however, we note there are now valuable templates to preregister secondary data analysis [40]).
Measures
CES-D-8
The eight-item version of the CES-D was administered at all nine waves [37]. The CES-D-8 is a shortened version of the CES-D 20-item self-report questionnaire [41]. It displays similar psychometric properties as the longer version in different populations, including adults aged 50 and above in Ireland [42] and adults aged 70 and above in the United States [37]. The scale assesses depressive symptoms from the previous week (Table 2 for item wording). The CES-D-8 uses a dichotomous response format instead of the original four response options to reduce participant burden and confusion, but this change does not affect the scale’s psychometric properties [37]. The dichotomous response format yields scores ranging from 0 (no symptoms) to 8 (all symptoms). The items happiness and enjoying life were reverse coded. Evidence for both a two and a one-factorial solution has been reported, including strict longitudinal invariance for both [43]. Items cover symptoms of depressed affect and somatic complaints, which constitute the factors of the two-factor solution.
Missingness
There was a high level of attrition among core sample members who participated in wave one (N = 11,391). Missingness rates peaked in wave nine at 70% (N = 3660). Little’s test for missingness [44] revealed that data were not missing completely at random, p < 0.001. Instead, sample characteristics predicted missingess: being non-white (vs. white), older, unmarried (vs. married), having a lower level of education, and greater depression severity, all p < 0.001 (consistent with [45]). This supports the assumption that data were missing depending on observed variables and are thus likely to be Missing at Random (MAR). Under this assumption, multiple imputation using these observed variables can help estimate unbiased parameters [46]. Given that network analysis is currently not compatible with multiple imputation methods, we only used one imputed dataset as recommended [47]. We imputed data by chained equations using the MICE package in R [48]. Given the binary responses, logistic regression was used for imputation [46]. In our imputation models, we included the variables associated with missingness as auxiliary variables.
Analysis strategy
We performed all analyses in R [49]. To examine temporal effects, we used CLPN modelling [47]. CLPN provides an ideal framework for our research question. It allows analysis of relationships between symptoms as directed paths over time in panel data with a few discrete measurement occasions (for an overview of other network modelling approaches and their application see [50]). Compared to cross-sectional networks, the directed paths in CLPNs indicate the symptom flow from one measurement occasion to a subsequent measurement occasion. These directed paths represent the shared variation between a symptom at time t and another symptom (either the same or different) at time t + 1, while accounting for all other symptoms at time t. We calculated the networks for consecutive timepoints, resulting in 8 network models (i.e., T1 → T2, T2 → T3, etc.). This way, we could compare the predictions of symptoms across different networks. Owing to the dichotomous response format of the CES-D-8, logistic regression models were used to compute autoregressive and cross-lagged coefficients. In autoregressive pathways, a symptom at one timepoint predicts itself at the next timepoint, adjusting for all other symptoms at the first timepoint. In the cross-lagged pathways, a symptom at one timepoint predicts a different symptom at the next timepoint, adjusting for all other symptoms at the first timepoint. We transformed the coefficients of the logistic regressions (i.e., edge weights) from log odds to odds ratios (ORs). This allows the interpretation of edge weights greater than 1 as a positive relationship and edge weights below 1 as a negative relationship; edge weights of 1 have no relationship. To estimate the regression coefficients, a penalized maximum likelihood with a lasso penalization was used [47]. A 10-fold cross-validation tuning parameter was applied so that small regression coefficients were set to zero [47]. We estimated the CLPN regressions using the glmnet package [51]. Gender and ethnicity were included as covariates as these were critical covariates in previous ELSA depression studies [52]. In addition, we ran cross-sectional network analysis on the nine-waves using the Ising model, which is able to handle binary data to compare the cross-sectional associations with the temporal associations [53].
We calculated the cross-lagged in-expected-influence and out-expected-influence as centrality indices [47]. In-expected-influence quantifies the degree to which each symptom is predicted by other symptoms in the network (the sum of the values of incoming edges associated with a symptom). Out-expected-influence describes the degree to which each symptom predicts other symptoms in the network (the sum of the values of outgoing edges associated with a symptom). To compare the networks across time, we compared the number of replicated edges across networks. In addition, we calculated the correlation among edge weights and centrality indices across networks [47].
The accuracy of edge weights was estimated by computing 95% confidence intervals (CIs) around each edge weight with nonparametric bootstrapping with 1000 iterations. To estimate the stability of our results, we used case-drop bootstrapping (correlating the centrality indices from the entire sample with centrality indices estimates on subsets of the sample) using the bootnet package with 1000 iterations [54]. In addition, we used the edge weight difference test and centrality difference test to pinpoint whether edges and centrality indices differ from each other significantly. The former test quantifies whether specific cross-lagged symptom connections (i.e., edges) are more important than other cross-lagged symptom connections. Likewise, the latter test quantifies whether some symptoms are more important (i.e., central) in the networks than other symptoms.
Results
Descriptive item-level statistics can be found in Table 2. Overall, restless sleep had the highest endorsement across all nine waves (following reverse coding of being happy and enjoying life). Endorsement of feeling depressed decreased over time and endorsement of enjoying life and happiness increased over time (p < 0.001), while the other items showed inconsistent fluctuations (Table 2). The networks exhibited good accuracy, as evidenced by edge weights with small to moderate bootstrapped CIs (supplemental Figs. s4-s11) [54]. All eight networks showed strong stability of the centrality measures as evidenced by case-drop bootstrapping results (supplemental Figs. s12-s19).
Longitudinal network comparisons
Networks were consistent over time. We observed strong correlations between cross-symptom coefficients in the networks (i.e., edge weight correlations, r = 0.73 – 0.98). Correlations were also strong across networks for both how much each symptom predicted other symptoms in the network and how much each symptom was predicted by other symptoms (out-expected-influence r = 0.55 – 0.92 and in-expected-influence 0.88 – 0.98, respectively). Further, consistency in the association of symptoms over time was demonstrated by cross-network replication of 80.3% – 91.7% of the edges in the networks. The cross-sectional networks of the nine waves revealed converging patterns of association compared to the temporal networks (Supplemental Figs. s2 and s3).
Autoregressive and cross-lagged edges
Figure 1 shows the eight CLPN models for all consecutive timepoints, depicting only coefficients where a symptom predicted another symptom (cross-lagged effects). When looking at the effects of symptoms on themselves over time (autoregressive pathways), loneliness exhibited the strongest autoregressive effect across all nine waves (OR: 6.33–9.33, Supplemental Material 3, Supplemental Figs. 1), with restless sleep (OR: 4.18–6.15) generally demonstrating the second highest autoregressive effect.
In four out the eight CLPN models, everything was an effort → could not get going displayed the strongest cross-lagged edges (OR: 1.80–2.33). In the other networks, this cross-lagged edge was at least among the top three strongest edges (OR: 1.94–2.10). Also, across waves these symptoms displayed significant cross-lagged edges in the opposite direction (could not get going → everything was an effort; range OR: 1.51–0.2.32). Moreover, a significant cross-lagged edge was found for everything was an effort → feeling depressed in all networks (OR: 1.45–2.12). Another consistent cross-lagged edge (edge rank position 1–9 across networks) was loneliness → feeling depressed (range OR: 1.64–2.34). Also, loneliness → sadness (OR: 1.47–2.20) displayed significant edge connections across all waves expect wave 8 → 9 network (OR: 1.20). The edges loneliness → everything was an effort (range OR: 1.35–1.97) had significant connections in all networks apart from the wave 7 → 8 network (OR: 1.15). Everything was an effort → loneliness (range OR: 1.24–2.21) had significant connections for all waves. Enjoying life → happiness (range OR: 1.62–2.14) and happiness → enjoying life (range OR: 1.23–2.03) displayed significant connections across all waves apart from the wave 3 → 4 network and the wave 2 → 3 network (both OR: 1.00). Edge weights difference tests for all networks indicated that the aforementioned edges (apart from the exceptions) were significantly stronger (p < 0.05) than most other edges across waves (supplemental Figs. s20-s27).
Note. Dep = felt depressed, Eft = everything you did was an effort, slp = restless sleep, hyp = happy, lnl = lonely, enj = enjoyed life, sad = felt sad, gng = could not get going. Arrows represent unique longitudinal relationships. Green edges indicate positive relationships; red edges indicate negative relationships (note that there are negative relationships as happy and enjoyed life were coded in the opposite direction as the other items). Edge thickness displays the relationship strength. Autoregressive edges and covariates were excluded to enhance visual interpretation. Yellow nodes represent symptoms of “depressed affect”. Blue nodes represent symptoms of “somatic complaints”. We used these factors according to the two-factor solution of the CES-D-8. Non-significant cross-lagged paths are excluded. All networks were visualized with an average layout using the qgraph package [77]. Nodes represent symptoms and arrows represent estimates of cross-lagged effects. The color of the arrows represents the directionality of the effect (green = positive effect, red = negative effect). Thicker arrows indicate stronger effects; non-significant cross-lagged paths were excluded. Nodes that cluster more strongly are placed together in the graph [78]. For better visual interpretation, nodes were colored according to the two-factorial solution of the CES-D-8 scale (depressed affect & somatic complaints). The underlying algorithm visualizes line thickness as a function of the strongest paths. For a better visual interpretation of the cross-lagged paths, we plotted networks in which only the cross-lagged effects are shown [47]. Bivariate connections among all symptoms over time (i.e., edge lists) are found in Supplement 2.
Centrality
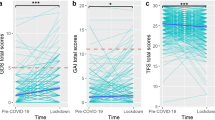
Figure 2 depicts the standardized centrality measures. Across waves, feeling depressed, everything was an effort, and could not get going had the strongest incoming connections (i.e., in-expected-influence). As can be seen in the eight difference plots in the supplement (Figs. s28 – s35), these symptoms had significantly greater (p < .05) in-expected-influence compared with most other symptoms. The symptoms loneliness and being sad also showed relatively high in-expected-influence. The lowest in-expected-influence emerged for the two reverse coded symptoms not being happy and not enjoying life. They showed significantly lower in-expected-influence compared to the other symptoms.
For outgoing connections (i.e., the centrality measure out-expected influence), the symptoms showed more variability across waves. Feeling depressed showed relatively low values. Everything was an effort, could not get going and loneliness were consistently among the symptoms with the strongest out-expected-influence. Difference plots in supplemental Figs. s32 to s40 show that these symptoms had higher values than many symptoms across time. At some but not all waves restless sleep had a high out-expected-influence especially at the wave 1 → wave 2 network (Fig. 2). Apart from two networks, happiness and enjoying life had low out-expected-influence across waves and thus most symptoms displayed significantly higher values across waves (Figs. s36-s43).
Summary of key findings
The findings can be summarized as follows. The associations between symptoms remained consistent over time. Everything was an effort and could not get going displayed strong temporal relationships with each other. They also strongly influenced other symptoms and were strongly influenced by other symptoms. In addition, loneliness influenced many other symptoms across time and especially itself. Feeling depressed was strongly influenced by other symptoms. Not being happy and not enjoying life had the lowest influence in the networks.
Discussion
This is the first study to examine longitudinal symptom constellations of depression in older adults ages 50 and above by computing separate CLPN covering a timespan of 16 years (mean ages 65 to 76 years). Networks exhibited consistency over time. This is important as network results are not always perfectly replicable over time [17, 18, 30]. While networks in the present study were not completely identical, we discuss the most robust similarities across networks as the minor differences between networks appeared to be random and cannot be meaningfully attributed to specific developmental windows.
The symptom feeling depressed had strong incoming connections but fewer outgoing connections, consistent with prior network studies [28, 38]. We also found sadness had relatively few outgoing edges, as found in a longitudinal treatment study of adults completing weekly assessments [31]. Thus, other symptoms (e.g., everything was an effort or loneliness) are more likely to lead to feeling depressed or sadness than vice versa. Findings in adolescent and adult populations are however mixed, and some studies report more outgoing connections of feeling depressed in longitudinal network analyses [30, 55]. These studies differ from the present study in either the age range studied (most were younger), time-lags between assessments (most were shorter), and depressive symptoms assessed (different scales were used). While it is difficult to tease apart the predominant factor contributing to these cross-study differences, feeling depressed may have fewer outgoing connections as a function of increasing age. Specifically, feeling depressed may constitute a reaction to life changes (e.g., bereavement, decreased mobility, more health-related issues) that are less prevalent for younger people. Our findings that feeling depressed appears to be activated by other symptoms yet lacks outgoing connections is of clinical relevance, as depressed mood is one out of two hallmark symptoms required for diagnosis [10]. However, according to network analysis findings including the present study [28, 32, 56], when depressed mood is present, other symptoms and associated impairment are likely to have been experienced for some time. Thus, these precursor symptoms may be an important focus of early intervention efforts.
For instance, the symptoms everything was an effort and could not get going displayed many incoming and outgoing connections and were also strongly associated with each other and with feeling depressed. These symptoms were thus core symptoms of our networks, which underscores the relevance of somatic symptoms in the context of depression among older people in line with research on symptom presentations of older adults (>65 years of age) diagnosed with depressive episodes [57]. These symptoms could reflect fatigue or increased burden, which could be initiated by bereavement, pain, or decreased mobility, and may activate a further depressive symptom cascade. Such symptoms could stem from diverse sources such as lack of energy, lack of motivation, feeling sick, unable to concentrate, or the presence of other medical conditions [6]. They may also reflect higher levels of apathy that are more common with older age and prevalent in later-life depression [58]. This may reflect some disengagement from society and aligns with our finding that everything was an effort displayed strong bidirectional relationships with loneliness. Social support is important throughout the life course and may be crucial to master daily tasks when growing older [59]. Therefore, higher levels of loneliness in older people may precede the feeling that everything was an effort. In the other direction, individuals may reduce their social contacts if meeting people is exhausting. This could enhance feelings of loneliness and thus everything was an effort and loneliness could be mutually reinforcing.
Overall, loneliness was an important symptom with many incoming and outgoing connections, and strongly predicted itself over time. This supports the observation that older people are often socially isolated [6]. As discussed above, loneliness can be increased by physical symptoms unrelated to depression in older adults [60]. The outgoing connections towards feeling depressed or sadness accord with previous research that loneliness in older adults predicted total scores of depressive symptoms one year later [61]. To extend our knowledge of loneliness in older adulthood, this symptom should be investigated in the context of separation, bereavement, and widowhood [62]. In addition, future work should scrutinize whether this symptom’s centrality differs as a function of feeling lonely versus being isolated due to one’s circumstances. In the broader literature, loneliness emerged as core symptom in adolescent depression networks [63,64,65,66] and was strongly associated with depressed affect in adults [67]. This suggests that loneliness is a core experience that leads to increased vulnerability to depression across the life course [6, 66, 68,69,70]. Sensitivity to social exclusion and the need for social connection appear to be fundamentally linked to depression across different developmental periods [34, 69, 71].
At most waves, restless sleep displayed outgoing connections but fewer incoming associations, in line with the only prior longitudinal network study in older adults where trouble sleeping had some outgoing connections but almost no incoming associations [28]. This item also strongly predicted itself over time. Results regarding this symptom were mixed in previous cross-sectional samples of older adults which could not disentangle incoming and outgoing connections [26]. As restless sleep can capture a variety of sleep difficulties (e.g., insomnia, parasomnia, restless leg syndrome), this symptom needs clarification in future studies. Within our network perspective, the overarching term restless sleep seemed to contribute to everything was an effort and could not get going, which, in turn, contributed to feeling depressed. This result aligns with a somatic pathway to depressive symptoms in older populations [8], and the association of disrupted sleep with the course of depression and treatment outcomes [36]. Restless sleep could be a potential warning symptom of depression in older adults, useful in primary prevention interventions [6]. However, this may not be specific to depression as restless sleep is considered a precursor to many forms of psychopathology [35].
Not enjoying life and not being happy [6] were strongly correlated with each other but were the least central symptoms on both centrality measures, which could be a byproduct of the reverse coding of these items. Around 90% of participants endorsed these items, resulting in the restricted range of variance, which can influence network centrality. It is probable that a substantial proportion of the variance in enjoying life is accounted for by happiness, and vice versa. This would lead to limited unique variance in either item, thereby resulting in minimal associations between enjoying life and other symptoms when controlling for happiness, and vice versa. Furthermore, the high degree of conceptual overlap between the two items may also result in topological overlap [29].
Clinical implications
While network studies can inform of central symptoms to target for interventions, significant associations between symptoms may not be clinically meaningful for several reasons [32, 72]. First, as associations have been found in general populations, network studies must be conducted in clinical populations to discern whether such associations hold. Second, even in clinical populations it remains unknown whether intervening on these central elements would be associated with symptom improvement let alone alleviating functional impairment. In theory, targeting core symptoms in a network should reduce overall network connectivity, but this has yet to be examined. Third, there is no consensus on what effect sizes between symptoms in a network are considered clinically meaningful. While smaller effect sizes may be meaningful on a population level, larger effect sizes are likely necessary in clinical populations to counteract functional impairment associated with depressive symptoms [73].
Nonetheless, central symptoms that consistently emerged in our networks over time (everything was an effort, could not get going, loneliness) may be potential key targets to mitigate depression in older adults on a population level [72]. These findings are of particular importance given their consistency across multiple time periods, which suggests the existence of shared processes that may be targeted at various developmental stages. Importantly, none of these symptoms were measured in the only prior longitudinal depression network study on older adults which we are aware of [28]. As these symptoms are not specific to depression but occur in the context of multiple other mental and physical disorders, they may even constitute viable transdiagnostic targets. Everything was an effort and could not get going may be targeted through behavioral activation (e.g., encouraging people to engage in activities). Setting achievable goals and engaging in meaningful activities that align with an individual’s values and interests can help individuals overcome the sense of everything being an effort and increase their enjoyment in daily life. To prevent and counteract the effects of loneliness, interventions have been proposed at the individual level (e.g., increasing social skills or increasing opportunities for social interaction) and societal level (e.g., targeting structures in educational and institutional settings) [74]. Our research should therefore stimulate intervention studies that empirically test whether targeting these symptoms leads to overall symptom reduction.
Strengths & limitations
Our longitudinal network analyses contributes significantly to the literature by disentangling incoming and outgoing connections of depressive symptoms over nine waves in a representative sample of older adults.
Limitations are as follows. First, findings from CLPN analysis may be biased since stable individual differences (between-person effects) are not disaggregated from within-person effects [47]. Thus, our results solely indicate that individuals who have higher levels of core symptoms (e.g., could not get going) are more likely to endorse other symptoms at the next time point. However, this does not reveal whether individuals with higher core symptoms than usual will experience a subsequent increase in other symptoms. Disaggregation of within- and between-person variances is possible with multilevel vector autoregression networks models in the context of experience sampling studies [54]. However, for such analyses to adequately capture within-person associations, many more waves of data are required than available in the present study. Furthermore, interpretation of these more complex models can be challenging [61], and in the absence of a control group, conclusions that one symptom causes another symptom to change are unfounded. Second, the present two-year time frame between assessments may occlude some shorter-term associations between symptoms. The level of symptom fluctuation within these two years is unknown and at the point of assessment we cannot discern whether the networks reflect cumulative change over two years or random fluctuations. However, the consistency of the results across networks over time points to enduring patterns of symptom prediction. Nonetheless, studies with shorter time-intervals, for example in the context of typical diagnostic measures (i.e., two weeks), or even on a daily basis, are desirable to capture finer-grained associations over time. Third, CES-D-8 only measures eight depressive symptoms, which are not exhaustive of this condition [75]. Core concepts like loneliness, somatic symptoms, or sleep problems were not captured in their entire breath which may have obfuscated more nuanced insights into the interrelatedness of these symptoms. Fourth, items were assessed with a dichotomous response format, potentially restricting their variance, which may have led to weaker associations among items than a continuous response format. Fifth, attrition was substantial in our sample. While we included variables associated with missingness in our imputation model, unmeasured variables may have contributed to attrition. Our imputed data are only unbiased if our data are missing at random [46]. Finally, the present contribution is limited to the ethnically white majority population of England [76]. This limitation is further compounded by the fact that ethnic minority status predicted study dropout.
Conclusion
The present study illuminates consistent longitudinal relationships between depressive symptoms in people 50 years and older. Everything was an effort, could not get going and loneliness emerged as key symptoms, which may serve as a starting point for further network analyses or intervention studies.
Data availability
Data are openly available to researchers via the UK Data Service.
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Volkert J, Schulz H, Härter M, Wlodarczyk O, Andreas S. The prevalence of mental disorders in older people in Western countries–a meta-analysis. Ageing Res Rev. 2013;12:339–53.
Hu T, Zhao X, Wu M, Li Z, Luo L, Yang C, et al. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res. 2022;311:114511.
Abdoli N, Salari N, Darvishi N, Jafarpour S, Solaymani M, Mohammadi M, et al. The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;132:1067–73.
Herrman H, Patel V, Kieling C, Berk M, Buchweitz C, Cuijpers P, et al. Time for united action on depression: a Lancet–World Psychiatric Association Commission. Lancet. 2022;399:957–1022.
Reynolds CF, Jeste DV, Sachdev PS, Blazer DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. 2022;21:336–63.
Barry LC, Abou JJ, Simen AA, Gill TM. Under-treatment of depression in older persons. J Affect Disord. 2012;136:789–96.
Schaakxs R, Comijs HC, Lamers F, Beekman ATF, Penninx B. Age-related variability in the presentation of symptoms of major depressive disorder. Psychol Med. 2017;47:543–52.
Korten NCM, Comijs HC, Lamers F, Penninx BWJH. Early and late onset depression in young and middle aged adults: Differential symptomatology, characteristics and risk factors? J Affect Disord. 2012;138:259–67.
American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013.947.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems (11th Revision). Retrieved from https://www.who.int/classifications/icd/en/ 2018.
Levecque K, Van Rossem R, De Boyser K, Van de Velde S, Bracke P. Economic hardship and depression across the life course: the impact of welfare state regimes. J Health Soc Behav. 2011;52:262–76.
Widaman KF, Revelle W. Thinking thrice about sum scores, and then some more about measurement and analysis. Behav Res Methods. 2022;1–19.
Fried EI, Nesse RM, Zivin K, Guille C, Sen S. Depression is more than the sum score of its parts: individual DSM symptoms have different risk factors. Psychol Med. 2014;44:2067–76.
Lux V, Kendler KS. Deconstructing major depression: a validation study of the DSM-IV symptomatic criteria. Psychol Med. 2010;40:1679–90.
Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR* D study. J Affect Disord. 2015;172:96–102.
Borsboom D, Deserno MK, Rhemtulla M, Epskamp S, Fried EI, McNally RJ, et al. Network analysis of multivariate data in psychological science. Nat Rev Methods Prim. 2021;1:1–18.
McNally RJ. Network Analysis of Psychopathology: Controversies and Challenges. Annu Rev Clin Psychol. 2021;17:31–53.
Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121.
Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13.
Fried EI. Lack of Theory Building and Testing Impedes Progress in The Factor and Network Literature. Psychol Inq. 2020;31:271–88.
Henry TR, Robinaugh DJ, Fried EI. On the control of psychological networks. Psychometrika. 2022;87:188–213.
Wichers M, Riese H, Hodges TM, Snippe E, Bos FM. A Narrative Review of Network Studies in Depression: What Different Methodological Approaches Tell Us About Depression. Front Psychiatry. 2021;12. Available from: https://doi.org/10.3389/fpsyt.2021.719490.
Belvederi Murri M, Amore M, Respino M, Alexopoulos GS. The symptom network structure of depressive symptoms in late-life: results from a European population study. Mol Psychiatry. 2020;25:1447–56.
An MH, Park SS, You SC, Park RW, Park B, Woo HK, et al. Depressive symptom network associated with comorbid anxiety in late-life depression. Front Psychiatry. 2019;10:856.
Castellanos MÁ, Ausín B, Bestea S, González-Sanguino C, Muñoz M. A network analysis of major depressive disorder symptoms and age-and gender-related differences in people over 65 in a Madrid community sample (Spain). Int J Environ Res Public Health. 2020;17:8934.
Airaksinen J, Gluschkoff K, Kivimäki M, Jokela M. Connectivity of depression symptoms before and after diagnosis of a chronic disease: A network analysis in the U.S. Health and Retirement Study. J Affect Disord. 2020;266:230–4.
Savelieva K, Komulainen K, Elovainio M, Jokela M. Longitudinal associations between specific symptoms of depression: Network analysis in a prospective cohort study. J Affect Disord. 2021;278:99–106.
Fried EI, Cramer AO. Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspect Psychol Sci. 2017;12:999–1020.
Funkhouser CJ, Chacko AA, Correa KA, Kaiser AJE, Shankman SA. Unique longitudinal relationships between symptoms of psychopathology in youth: A cross-lagged panel network analysis in the ABCD study. J Child Psychol Psychiatry. 2021;62:184–94.
Bringmann LF, Lemmens LH, Huibers MJ, Borsboom D, Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol Med. 2015;45:747–57.
Bringmann LF, Albers C, Bockting C, Borsboom D, Ceulemans E, Cramer A, et al. Psychopathological networks: Theory, methods and practice. Behav Res Ther. 2022;149:104011.
Domènech-Abella J, Mundó J, Haro JM, Rubio-Valera M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J Affect Disord. 2019;246:82–8.
Donovan NJ, Blazer D. Social isolation and loneliness in older adults: review and commentary of a National Academies report. Am J Geriatr Psychiatry. 2020;28:1233–44.
Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. 2011;31:225–35.
Troxel WM, Kupfer DJ, Iii CFR, Frank E, Thase ME, Miewald JM, et al. Insomnia and Objectively Measured Sleep Disturbances Predict Treatment Outcome in Depressed Patients Treated With Psychotherapy or Psychotherapy-Pharmacotherapy Combinations. J Clin Psychiatry. 2011;72:9153.
Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11:139–48.
Malgaroli M, Calderon A, Bonanno GA. Networks of major depressive disorder: A systematic review. Clin Psychol Rev. 2021;85:102000.
Steptoe A, Breeze E, Banks J, Nazroo J. Cohort Profile: The English Longitudinal Study of Ageing. Int J Epidemiol. 2013;42:1640–8.
Akker OR van den, Weston S, Campbell L, Chopik B, Damian R, Davis-Kean P, et al. Preregistration of secondary data analysis: A template and tutorial. Meta-Psychol. 2021;5. Available from: https://open.lnu.se/index.php/metapsychology/article/view/2625.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Briggs R, Carey D, O’Halloran AM, Kenny RA, Kennelly SP. Validation of the 8-item Centre for Epidemiological Studies Depression Scale in a cohort of community-dwelling older people: data from The Irish Longitudinal Study on Ageing (TILDA). Eur Geriatr Med. 2018;9:121–6.
Schlechter P, Ford T, Neufeld S. The Eight-Item Center for Epidemiological Studies Depression Scale in the English Longitudinal Study of Aging: Longitudinal and Gender Invariance, Sum Score Models, and External Associations. Assessment. 2022;10731911221138930.
Little RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–202.
White J, Zaninotto P, Walters K, Kivimäki M, Demakakos P, Biddulph J, et al. Duration of depressive symptoms and mortality risk: The English Longitudinal Study of Ageing (ELSA). Br J Psychiatry. 2016;208:337–42.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–99.
Wysocki A, Rhemtulla M, Bork R van, Cramer A. Cross-Lagged Network Models. PsyArXiv; 2022. Available from: https://psyarxiv.com/vjr8z/.
van Buuren S, Groothuis-Oudshoorn K, Robitzsch A, Vink G, Doove L, Jolani S. Package ‘mice.’ Comput Softw. 2015.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2012. 2021.
Epskamp S, Waldorp LJ, Mõttus R, Borsboom D. The Gaussian Graphical Model in Cross-Sectional and Time-Series Data. Multivar Behav Res. 2018;53:453–80.
Friedman JH, Hastie T, Tibshirani R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J Stat Softw. 2010;33:22.
Blöchl M, Schaare HL, Kunzmann U, Nestler S. The Age-Dependent Association Between Vascular Risk Factors and Depressed Mood. J Gerontol Ser B. 2022;77:284–94.
Altenbuchinger M, Weihs A, Quackenbush J, Grabe HJ, Zacharias HU. Gaussian and Mixed Graphical Models as (multi-) omics data analysis tools. Biochim Biophys Acta BBA-Gene Regul Mech. 2020;1863:194418.
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. 2018;50:195–212.
Bernstein EE, Kleiman EM, van Bork R, Moriarity DP, Mac Giollabhui N, McNally RJ, et al. Unique and predictive relationships between components of cognitive vulnerability and symptoms of depression. Depress Anxiety. 2019;36:950–9.
Fisher AJ, Reeves JW, Lawyer G, Medaglia JD, Rubel JA. Exploring the idiographic dynamics of mood and anxiety via network analysis. J Abnorm Psychol. 2017;126:1044–56.
Wilkowska-Chmielewska J, Szelenberger W, Wojnar M. Age-dependent symptomatology of depression in hospitalized patients and its implications for DSM-5. J Affect Disord. 2013;150:142–5.
Mehta M, Whyte E, Lenze E, Hardy S, Roumani Y, Subashan P, et al. Depressive symptoms in late life: associations with apathy, resilience and disability vary between young-old and old-old. Int J Geriatr Psychiatry. 2008;23:238–43.
Wu F, Sheng Y. Social support network, social support, self-efficacy, health-promoting behavior and healthy aging among older adults: A pathway analysis. Arch Gerontol Geriatr. 2019;85:103934.
Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkälä KH. Predictors and subjective causes of loneliness in an aged population. Arch Gerontol Geriatr. 2005;41:223–33.
Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453.
Pan H, Liu Q. Difference of depression between widowed and non-widowed older people in China: A network analysis approach. J Affect Disord. 2021;280:68–76.
Gijzen MWM, Rasing SPA, Creemers DHM, Smit F, Engels RCME, De Beurs D. Suicide ideation as a symptom of adolescent depression. a network analysis. J Affect Disord. 2021;278:68–77.
Kim D, Kwon HJ, Ha M, Lim MH, Kim KM. Network analysis for the symptom of depression with Children’s Depression Inventory in a large sample of school-aged children. J Affect Disord. 2021;281:256–63.
Manfro PH, Pereira RB, Rosa M, Cogo-Moreira H, Fisher HL, Kohrt BA, et al. Adolescent depression beyond DSM definition: a network analysis. Eur Child Adolesc Psychiatry. 2021. Available from: https://doi.org/10.1007/s00787-021-01908-1.
Schlechter P, Ford T, Neufeld SA. Depressive symptom networks in the UK general adolescent population and in those looked after by local authorities. BMJ Ment Health. 2023;26. Available from: https://mentalhealth.bmj.com/content/26/1/e300707.abstract.
von Känel R, Weilenmann S, Spiller TR. Loneliness is associated with depressive affect, but not with most other symptoms of depression in community-dwelling individuals: a network analysis. Int J Environ Res Public Health. 2021;18:2408.
Achterbergh L, Pitman A, Birken M, Pearce E, Sno H, Johnson S. The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature. BMC Psychiatry. 2020;20:415.
Goossens L. Loneliness in Adolescence: Insights From Cacioppo’s Evolutionary Model. Child Dev Perspect. 2018;12:230–4.
Odenthal M, Schlechter P, Benke C, Pané-Farré CA. Temporal dynamics in mental health symptoms and loneliness during the COVID-19 pandemic in a longitudinal probability sample: a network analysis. Transl Psychiatry. 2023;13:1–9.
Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17:1–7.
Lunansky G, Naberman J, van Borkulo CD, Chen C, Wang L, Borsboom D. Intervening on psychopathology networks: Evaluating intervention targets through simulations. Methods. 2022;204:29–37.
Carey EG, Ridler I, Ford TJ, Stringaris A. Editorial Perspective: When is a ‘small effect’actually large and impactful? J Child Psychol Psychiatry. 2023.
Jeste DV, Lee EE, Cacioppo S. Battling the Modern Behavioral Epidemic of Loneliness: Suggestions for Research and Interventions. JAMA Psychiatry. 2020;77:553–4.
Fried EI, Flake JK, Robinaugh DJ. Revisiting the theoretical and methodological foundations of depression measurement. Nat Rev Psychol. 2022;1:358–68.
Chen FF. What happens if we compare chopsticks with forks? The impact of making inappropriate comparisons in cross-cultural research. J Pers Soc Psychol. 2008;95:1005.
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network Visualizations of Relationships in Psychometric Data. J Stat Softw. 2012;48:1–18.
Fruchterman TM, Reingold EM. Graph drawing by force-directed placement. Softw Pr Exp. 1991;21:1129–64.
Funding
PS was funded by the Cusanuswerk. SN was supported by the Cundill Centre for Child and Youth Depression and Wellcome Trust (Institutional Strategic Support Fund 204845/Z/16/Z, and Early Career Award 226392/Z/22/Z). TF received support from the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
PS played lead role in conceptualization, formal analysis, investigation, methodology, software, writing and editing of original draft. TJF played supporting role in supervision and editing the original draft. SASN played lead role in supervision, conceptualization, methodology and writing and editing of original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schlechter, P., Ford, T.J. & Neufeld, S.A.S. The development of depressive symptoms in older adults from a network perspective in the English Longitudinal Study of Ageing. Transl Psychiatry 13, 363 (2023). https://doi.org/10.1038/s41398-023-02659-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-023-02659-0