Abstract
Basal cell carcinoma (BCC) of the skin is the most common malignant neoplasm in humans. BCC is primarily driven by the Sonic Hedgehog (Hh) pathway. However, its phenotypic variation remains unexplained. Our genetic profiling of 293 BCCs found the highest mutation rate in cancer (65 mutations/Mb). Eighty-five percent of the BCCs harbored mutations in Hh pathway genes (PTCH1, 73% or SMO, 20% (P = 6.6 × 10−8) and SUFU, 8%) and in TP53 (61%). However, 85% of the BCCs also harbored additional driver mutations in other cancer-related genes. We observed recurrent mutations in MYCN (30%), PPP6C (15%), STK19 (10%), LATS1 (8%), ERBB2 (4%), PIK3CA (2%), and NRAS, KRAS or HRAS (2%), and loss-of-function and deleterious missense mutations were present in PTPN14 (23%), RB1 (8%) and FBXW7 (5%). Consistent with the mutational profiles, N-Myc and Hippo-YAP pathway target genes were upregulated. Functional analysis of the mutations in MYCN, PTPN14 and LATS1 suggested their potential relevance in BCC tumorigenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Iwasaki, J.K., Srivastava, D., Moy, R.L., Lin, H.J. & Kouba, D.J. The molecular genetics underlying basal cell carcinoma pathogenesis and links to targeted therapeutics. J. Am. Acad. Dermatol. 66, e167–e178 (2012).
Youssef, K.K. et al. Identification of the cell lineage at the origin of basal cell carcinoma. Nat. Cell Biol. 12, 299–305 (2010).
Hahn, H. et al. Mutations of the human homolog of Drosophila patched in the nevoid basal cell carcinoma syndrome. Cell 85, 841–851 (1996).
Reifenberger, J. et al. Somatic mutations in the PTCH, SMOH, SUFUH and TP53 genes in sporadic basal cell carcinomas. Br. J. Dermatol. 152, 43–51 (2005).
Sharpe, H.J. et al. Genomic analysis of Smoothened inhibitor resistance in basal cell carcinoma. Cancer Cell 27, 327–341 (2015).
Atwood, S.X. et al. Smoothened variants explain the majority of drug resistance in basal cell carcinoma. Cancer Cell 27, 342–353 (2015).
Smith, M.J. et al. Germline mutations in SUFU cause Gorlin syndrome–associated childhood medulloblastoma and redefine the risk associated with PTCH1 mutations. J. Clin. Oncol. 32, 4155–4161 (2014).
Sweeney, R.T. et al. Identification of recurrent SMO and BRAF mutations in ameloblastomas. Nat. Genet. 46, 722–725 (2014).
Laurendeau, I. et al. Gene expression profiling of the hedgehog signaling pathway in human meningiomas. Mol. Med. 16, 262–270 (2010).
Brastianos, P.K. et al. Genomic sequencing of meningiomas identifies oncogenic SMO and AKT1 mutations. Nat. Genet. 45, 285–289 (2013).
Pomeroy, S.L. et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature 415, 436–442 (2002).
Clark, V.E. et al. Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339, 1077–1080 (2013).
Jayaraman, S.S., Rayhan, D.J., Hazany, S. & Kolodney, M.S. Mutational landscape of basal cell carcinomas by whole-exome sequencing. J. Invest. Dermatol. 134, 213–220 (2014).
Basset-Seguin, N. et al. Vismodegib in patients with advanced basal cell carcinoma (STEVIE): a pre-planned interim analysis of an international, open-label trial. Lancet Oncol. 16, 729–736 (2015).
Von Hoff, D.D. et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N. Engl. J. Med. 361, 1164–1172 (2009).
Sekulic, A. et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N. Engl. J. Med. 366, 2171–2179 (2012).
Dreno, B., Basset-Seguin, N., Caro, I., Yue, H. & Schadendorf, D. Clinical benefit assessment of vismodegib therapy in patients with advanced basal cell carcinoma. Oncologist 19, 790–796 (2014).
Chang, A.L. & Oro, A.E. Initial assessment of tumor regrowth after vismodegib in advanced basal cell carcinoma. Arch. Dermatol. 148, 1324–1325 (2012).
Lawrence, M.S. et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 505, 495–501 (2014).
Hodis, E. et al. A landscape of driver mutations in melanoma. Cell 150, 251–263 (2012).
Cancer Genome Atlas Network. Genomic classification of cutaneous melanoma. Cell 161, 1681–1696 (2015).
Nikolaev, S.I. et al. Exome sequencing identifies recurrent somatic MAP2K1 and MAP2K2 mutations in melanoma. Nat. Genet. 44, 133–139 (2012).
Drobetsky, E.A. & Sage, E. UV-induced G:C-->A:T transitions at the APRT locus of Chinese hamster ovary cells cluster at frequently damaged 5′-TCC-3′ sequences. Mutat. Res. 289, 131–138 (1993).
Marionnet, C., Benoit, A., Benhamou, S., Sarasin, A. & Stary, A. Characteristics of UV-induced mutation spectra in human XP-D/ERCC2 gene–mutated xeroderma pigmentosum and trichothiodystrophy cells. J. Mol. Biol. 252, 550–562 (1995).
Alexandrov, L.B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013).
Hanawalt, P.C., Donahue, B.A. & Sweder, K.S. Repair and transcription. Collision or collusion? Curr. Biol. 4, 518–521 (1994).
Besaratinia, A., Kim, S.I., Bates, S.E. & Pfeifer, G.P. Riboflavin activated by ultraviolet A1 irradiation induces oxidative DNA damage–mediated mutations inhibited by vitamin C. Proc. Natl. Acad. Sci. USA 104, 5953–5958 (2007).
Brash, D.E. UV signature mutations. Photochem. Photobiol. 91, 15–26 (2015).
Hu, J., Adar, S., Selby, C.P., Lieb, J.D. & Sancar, A. Genome-wide analysis of human global and transcription-coupled excision repair of UV damage at single-nucleotide resolution. Genes Dev. 29, 948–960 (2015).
McGregor, J.M. et al. Spectrum of p53 gene mutations suggests a possible role for ultraviolet radiation in the pathogenesis of advanced cutaneous lymphomas. J. Invest. Dermatol. 112, 317–321 (1999).
da Silva Almeida, A.C. et al. The mutational landscape of cutaneous T cell lymphoma and Sézary syndrome. Nat. Genet. 47, 1465–1470 (2015).
Strano, S. et al. Mutant p53: an oncogenic transcription factor. Oncogene 26, 2212–2219 (2007).
Kato, G.J. & Dang, C.V. Function of the c-Myc oncoprotein. FASEB J. 6, 3065–3072 (1992).
Bahram, F., von der Lehr, N., Cetinkaya, C. & Larsson, L.G. c-Myc hot spot mutations in lymphomas result in inefficient ubiquitination and decreased proteasome-mediated turnover. Blood 95, 2104–2110 (2000).
Welcker, M. et al. The Fbw7 tumor suppressor regulates glycogen synthase kinase 3 phosphorylation-dependent c-Myc protein degradation. Proc. Natl. Acad. Sci. USA 101, 9085–9090 (2004).
Freier, K. et al. Recurrent NMYC copy number gain and high protein expression in basal cell carcinoma. Oncol. Rep. 15, 1141–1145 (2006).
Stacey, S.N. et al. New basal cell carcinoma susceptibility loci. Nat. Commun. 6, 6825 (2015).
Knoepfler, P.S. & Kenney, A.M. Neural precursor cycling at sonic speed: N-Myc pedals, GSK-3 brakes. Cell Cycle 5, 47–52 (2006).
Wong, Y.H. et al. KinasePhos 2.0: a web server for identifying protein kinase–specific phosphorylation sites based on sequences and coupling patterns. Nucleic Acids Res. 35, W588–W594 (2007).
Wang, W. et al. PTPN14 is required for the density-dependent control of YAP1. Genes Dev. 26, 1959–1971 (2012).
Welcker, M. & Clurman, B.E. FBW7 ubiquitin ligase: a tumour suppressor at the crossroads of cell division, growth and differentiation. Nat. Rev. Cancer 8, 83–93 (2008).
King, B. et al. The ubiquitin ligase FBXW7 modulates leukemia-initiating cell activity by regulating MYC stability. Cell 153, 1552–1566 (2013).
Zhang, H., Pasolli, H.A. & Fuchs, E. Yes-associated protein (YAP) transcriptional coactivator functions in balancing growth and differentiation in skin. Proc. Natl. Acad. Sci. USA 108, 2270–2275 (2011).
Schlegelmilch, K. et al. Yap1 acts downstream of α-catenin to control epidermal proliferation. Cell 144, 782–795 (2011).
Wilson, K.E. et al. PTPN14 forms a complex with Kibra and LATS1 proteins and negatively regulates the YAP oncogenic function. J. Biol. Chem. 289, 23693–23700 (2014).
Hao, Y., Chun, A., Cheung, K., Rashidi, B. & Yang, X. Tumor suppressor LATS1 is a negative regulator of oncogene YAP. J. Biol. Chem. 283, 5496–5509 (2008).
Tate, G., Kishimoto, K. & Mitsuya, T. Biallelic alterations of the large tumor suppressor 1 (LATS1) gene in infiltrative, but not superficial, basal cell carcinomas in a Japanese patient with nevoid basal cell carcinoma syndrome. Med. Mol. Morphol. 48, 177–182 (2015).
Krauthammer, M. et al. Exome sequencing identifies recurrent somatic RAC1 mutations in melanoma. Nat. Genet. 44, 1006–1014 (2012).
Hammond, D. et al. Melanoma-associated mutations in protein phosphatase 6 cause chromosome instability and DNA damage owing to dysregulated Aurora-A. J. Cell Sci. 126, 3429–3440 (2013).
Duman-Scheel, M., Weng, L., Xin, S. & Du, W. Hedgehog regulates cell growth and proliferation by inducing cyclin D and cyclin E. Nature 417, 299–304 (2002).
Stefansson, B. & Brautigan, D.L. Protein phosphatase PP6 N terminal domain restricts G1 to S phase progression in human cancer cells. Cell Cycle 6, 1386–1392 (2007).
Couzens, A.L. et al. Protein interaction network of the mammalian Hippo pathway reveals mechanisms of kinase-phosphatase interactions. Sci. Signal. 6, rs15 (2013).
Jaju, P.D. et al. Mutations in the kinetochore gene KNSTRN in basal cell carcinoma. J. Invest. Dermatol. 135, 3197–3200 (2015).
Lee, C.S. et al. Recurrent point mutations in the kinetochore gene KNSTRN in cutaneous squamous cell carcinoma. Nat. Genet. 46, 1060–1062 (2014).
Santos, G.C., Zielenska, M., Prasad, M. & Squire, J.A. Chromosome 6p amplification and cancer progression. J. Clin. Pathol. 60, 1–7 (2007).
Zhang, H. et al. TEAD transcription factors mediate the function of TAZ in cell growth and epithelial-mesenchymal transition. J. Biol. Chem. 284, 13355–13362 (2009).
Valentijn, L.J. et al. Functional MYCN signature predicts outcome of neuroblastoma irrespective of MYCN amplification. Proc. Natl. Acad. Sci. USA 109, 19190–19195 (2012).
Pfister, S. et al. Outcome prediction in pediatric medulloblastoma based on DNA copy-number aberrations of chromosomes 6q and 17q and the MYC and MYCN loci. J. Clin. Oncol. 27, 1627–1636 (2009).
Xu, L. et al. Sonic Hedgehog pathway is essential for neuroblastoma cell proliferation and tumor growth. Mol. Cell. Biochem. 364, 235–241 (2012).
Oue, T., Yoneda, A., Uehara, S., Yamanaka, H. & Fukuzawa, M. Increased expression of the hedgehog signaling pathway in pediatric solid malignancies. J. Pediatr. Surg. 45, 387–392 (2010).
Murphy, A.J. et al. Aberrant activation, nuclear localization, and phosphorylation of Yes-associated protein-1 in the embryonic kidney and Wilms tumor. Pediatr. Blood Cancer 61, 198–205 (2014).
Pugh, T.J. et al. The genetic landscape of high-risk neuroblastoma. Nat. Genet. 45, 279–284 (2013).
Ellison, D.W. et al. Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathol. 121, 381–396 (2011).
Williams, R.D. et al. Multiple mechanisms of MYCN dysregulation in Wilms tumour. Oncotarget 6, 7232–7243 (2015).
Nikolaev, S.I. et al. Frequent cases of RAS-mutated Down syndrome acute lymphoblastic leukaemia lack JAK2 mutations. Nat. Commun. 5, 4654 (2014).
Vogelstein, B. et al. Cancer genome landscapes. Science 339, 1546–1558 (2013).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
Nikolaev, S. et al. Extrachromosomal driver mutations in glioblastoma and low-grade glioma. Nat. Commun. 5, 5690 (2014).
Mermel, C.H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, R41 (2011).
Lawrence, M.S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013).
Roadmap Epigenomics Consortium. Integrative analysis of 111 reference human epigenomes. Nature 518, 317–330 (2015).
Chen, C.L. et al. Impact of replication timing on non-CpG and CpG substitution rates in mammalian genomes. Genome Res. 20, 447–457 (2010).
Cancer Genome Atlas Network. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517, 576–582 (2015).
Nikolayeva, O. & Robinson, M.D. edgeR for differential RNA-seq and ChIP-seq analysis: an application to stem cell biology. Methods Mol. Biol. 1150, 45–79 (2014).
Huang, W., Sherman, B.T. & Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 4, 44–57 (2009).
Huang, W., Sherman, B.T. & Lempicki, R.A. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 37, 1–13 (2009).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA 102, 15545–15550 (2005).
Buchan, D.W., Minneci, F., Nugent, T.C., Bryson, K. & Jones, D.T. Scalable web services for the PSIPRED Protein Analysis Workbench. Nucleic Acids Res. 41, W349–W357 (2013).
Dinkel, H. et al. The eukaryotic linear motif resource ELM: 10 years and counting. Nucleic Acids Res. 42, D259–D266 (2014).
Eswar, N. et al. Comparative protein structure modeling using MODELLER. Curr. Protoc. Protein Sci. Chapter 2, Unit 2.9 (2007).
Guerois, R., Nielsen, J.E. & Serrano, L. Predicting changes in the stability of proteins and protein complexes: a study of more than 1000 mutations. J. Mol. Biol. 320, 369–387 (2002).
Lodrini, M. et al. MYCN and HDAC2 cooperate to repress miR-183 signaling in neuroblastoma. Nucleic Acids Res. 41, 6018–6033 (2013).
Xiao, W. et al. Mutual interaction between YAP and c-Myc is critical for carcinogenesis in liver cancer. Biochem. Biophys. Res. Commun. 439, 167–172 (2013).
Li, L. et al. MEK1 promotes YAP and their interaction is critical for tumorigenesis in liver cancer. FEBS Lett. 587, 3921–3927 (2013).
Gerdes, J., Becker, M.H., Key, G. & Cattoretti, G. Immunohistological detection of tumour growth fraction (Ki-67 antigen) in formalin-fixed and routinely processed tissues. J. Pathol. 168, 85–86 (1992).
Acknowledgements
We thank Z. Modrusan (next-generation sequencing), R. Piskol (computational biology), G. Pau (computational biology), F. Peale (pathology) and S. Jillo (collaboration management) from Genentech, Inc. This work was supported by Swiss Cancer League (LSCC 2939-02-2012), Dinu Lipatti 2014 and Novartis (14B065) research grants to S.I.N.
Author information
Authors and Affiliations
Contributions
S.I.N. and L.P. designed the project. S.I.N. and X.B. performed high-throughput sequencing data analysis. S.I.N., F.B., K.P., F.A.S. and R.B.C. performed statistical analysis. S.I.N., X.B., H.J.S., F.J.d.S. and S.E.A. wrote the manuscript. V.Z. and O.M. performed in silico modeling. X.B. and P.G.R. performed sample and high-throughput sequencing library preparation. L.P., N.B.-S., G.K. and K.G. collected samples. B.K. and I.A. performed MYCN in vivo experiments. T.M. and C.V. performed PTPN14 immunohistochemistry experiments. S.I.N., A.L. and M. Garieri performed RNA-seq analysis. V.B.S., M.A.A. and S.I.N. performed mutational signature analysis. M. Guipponi, P.G.R. and X.B. performed exome capture and high-throughput sequencing. M.E. and O.S. performed experiments.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Mutational signatures in BCC compared to melanoma.
(a) The effect of transcription-coupled repair as a function of gene expression in BCC. Tumor type–specific gene expression levels were used for BCC (this study) and cutaneous melanoma21. Genes were grouped into five equally sized bins by their level of expression. 95% confidence intervals for the ratio between the two binomial distributions were calculated using the R function riskscoreci(). (b) Fraction of each nucleotide 5′ to C>A mutations.
Supplementary Figure 2 Distribution of mutations in BCC driver genes.
(a–n) Distribution of mutations in the full sample set (293 BCC samples) along the FBXW7 (a), PPP6C (b), STK19 (c), CASP8 (d), RB1 (e), KNSTRN (f), ERBB2 (g), NOTCH2 (h), NOTCH1 (i), ARID1A (j), SMO (k), TP53 (l), PTCH1 (m) and SUFU (n) protein diagrams. The orange lollipops represent truncating mutations, the purple lollipops represent missense mutations and the blue lollipops represent both truncating and missense events affecting the same amino acid. Protein functional domains are represented by colored boxes. The most recurrent events for each protein are labeled with the amino acid change. Protein diagrams were generated with cBioPortal tools.
Supplementary Figure 3 SCNAs in BCC exomes.
Top, overall profile of SCNAs in BCC. LOHs and cnLOHs are on the top (dark blue); amplified regions are on the bottom (red). The positions of relevant genes are marked. Bottom, per-tumor SCNA profile. Each line represents a sample, and each column represents a chromosome. Loss of an allele (LOH) is depicted in blue, cnLOH is indicated in black and copy number gain is indicated in yellow. Chromosomes X and Y have been excluded.
Supplementary Figure 4 LATS2 mutations in BCC.
(a) Distribution of mutations (in the 136 sequenced exomes only) along the LATS2 protein schema. The purple lollipops represent missense mutations, and the orange lollipops represent truncating mutations. Protein functional domains are represented by green boxes. Events occurring two or more times are labeled with the amino acid change. (b) Kinase domain structure of LATS2 highlighting the position of residue Pro1004. The protein diagram was generated with cBioPortal tools.
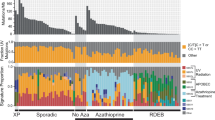
Supplementary Figure 5 Fraction of tumors with driver mutations per category.
The bars represent the fraction of samples with driver mutations per BCC category indicated in the header (only non-clonal samples were used in this analysis). Vismo, vismodegib. Genes harboring driver mutations are labeled on the x axis. MYCN-p.44 is a subcategory containing only tumors with MYCN p.44 mutations; PTPN14-tr corresponds to PTPN14 truncating mutations. The fraction of tumors represented by the bars can be found at the left.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–5 and Supplementary Note. (PDF 1459 kb)
Supplementary Table 1
Sample characteristics and sequencing statistics. (XLSX 121 kb)
Supplementary Table 2
Cancer panel genes. (XLSX 13 kb)
Supplementary Table 3
Somatic mutations identified in exome and cancer panel sequenced samples. (XLSX 40169 kb)
Supplementary Table 4
Fraction of mutations on the transcribed strand. (XLSX 9 kb)
Supplementary Table 5
MutSigCV analysis of cancer panel genes on exome-sequenced tumors (121 samples). (XLSX 2197 kb)
Supplementary Table 6
TumOnc output for cancer panel genes on the full data set (non-clonal tumors). (XLSX 21 kb)
Supplementary Table 7
Fraction of tumor cells and fraction of UV light–induced mutations per sample. (XLSX 23 kb)
Supplementary Table 8
Somatic copy number aberrations (SCNAs). (XLSX 33 kb)
Rights and permissions
About this article
Cite this article
Bonilla, X., Parmentier, L., King, B. et al. Genomic analysis identifies new drivers and progression pathways in skin basal cell carcinoma. Nat Genet 48, 398–406 (2016). https://doi.org/10.1038/ng.3525
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3525